Next-Generation Microbiome Medicine Could Change How Parkinson’s Disease Is Treated

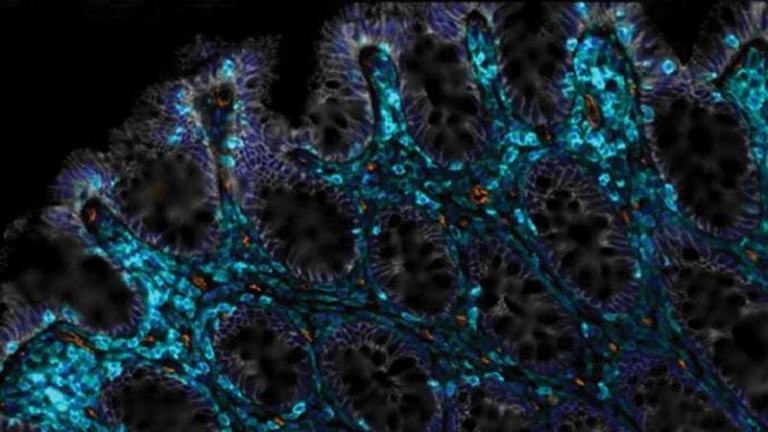
Researchers at the University of Georgia’s College of Veterinary Medicine have developed a bioengineered probiotic that might completely reshape how we treat Parkinson’s disease and other neurological disorders. This new approach uses a modified strain of the well-known probiotic Escherichia coli Nissle 1917 to produce a steady stream of levodopa (L-DOPA) directly inside the gut. Because levodopa has long been the gold-standard drug for Parkinson’s disease, delivering it in a more stable way could address major challenges patients face with current treatments.
The research was led by Anumantha Kanthasamy, a professor and director of the Isakson Center for Neurological Disease Research (ICNDR). His team includes multiple scientists such as Gregory Phillips and Piyush Padhi, all working together across microbiology, neuropharmacology, pathology, infectious diseases, and statistics. Their findings were published in Cell Host & Microbe, and the implications are genuinely exciting.
A Probiotic Re-Engineered to Make Medicine
The engineered microbe is based on E. coli Nissle 1917, a strain that has been safely used in humans for more than a century. This safety record made it an ideal candidate for modification.
The team inserted a genetic pathway into the bacterium enabling it to continuously synthesize levodopa from naturally available substances in the gut. Once produced, levodopa can travel through the bloodstream and eventually reach the brain, where it converts into dopamine. This neurotransmitter is essential for movement and is severely depleted in people with Parkinson’s disease.
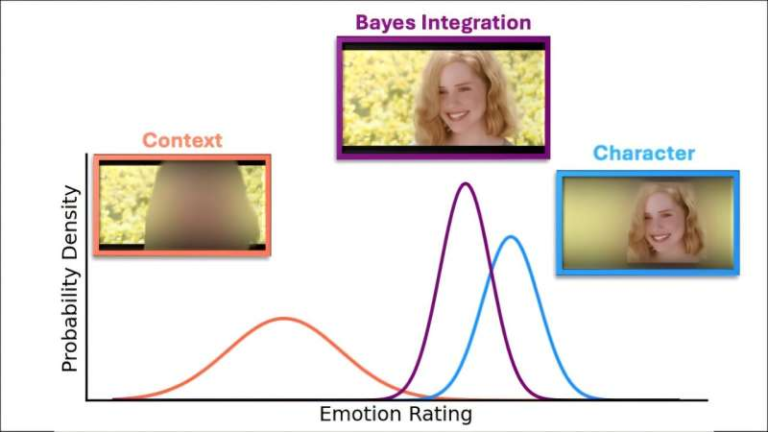
What makes the innovation especially promising is its steady, sustained delivery. Instead of patients relying on pills taken multiple times a day—each producing spikes and drops in dopamine—the engineered microbe releases levodopa in a more continuous pattern. This could help prevent complications caused by fluctuating drug levels.
Why Parkinson’s Patients Need a Better Delivery System
Parkinson’s disease develops as dopamine-producing neurons in the brain gradually deteriorate. Standard treatment relies on oral levodopa, a drug that has remained unmatched in its ability to relieve symptoms such as slow movement, tremors, rigidity, and balance problems.
But despite being effective, oral levodopa has a major drawback:
Its effects rise and fall inconsistently.
When levodopa enters the bloodstream in waves, brain dopamine levels swing up and down. These fluctuations can cause dyskinesia, which includes involuntary movements of the limbs, face, neck, and torso. Dyskinesia often gets mistaken for a symptom of the disease, but it actually stems from the medication itself.
The new probiotic-based treatment aims to solve this by creating a continuous supply of levodopa from the gut. With fewer peaks and troughs, patients may experience:
- More stable motor control
- Fewer medication-related side effects
- Reduced dependence on multiple daily doses
- Improved quality of life
If successful in humans, this would be the first noninvasive, sustained, live biotherapeutic delivery of levodopa.
How the Engineered Probiotic Works
According to the research, the team genetically modified the bacterium to produce levodopa using built-in metabolic machinery. This living drug is designed to:
- Survive inside the human gut
- Respond to environmental cues
- Produce levodopa continuously
- Release it in a controlled manner
This concept is part of a growing movement in synthetic biology: turning microbes into tiny, living drug factories.
Padhi, one of the lead researchers, explained that gut microbes naturally act as chemical processors. They produce metabolites all the time, so why not engineer them to produce something medically useful? In this case, that “something” is levodopa—delivered in a way that avoids the unstable dosing patterns of pills.
Preclinical Evidence and Next Steps
The research team tested their bioengineered microbe in several preclinical models, and the results were promising. The probiotic improved motor function and maintained steady levodopa levels, which is difficult to achieve with standard pills.
The project was a major collaboration between:
- Physiology and Pharmacology
- Pathology
- Infectious Diseases
- The Department of Statistics
Early phases were conducted at Iowa State University’s College of Veterinary Medicine before moving to UGA.
Based on the animal studies, the researchers believe the therapy is ready for human clinical trials. If approved, these trials could determine how the probiotic colonizes the human gut, how long its effects last, and how safe it is in long-term use.
Kanthasamy notes that the platform could eventually expand to treat not only Parkinson’s disease but also other conditions requiring continuous neurochemical support, including Alzheimer-related dementia.
Why the Gut–Brain Connection Matters
The idea of using the gut to treat neurological disorders isn’t random; it’s based on a rapidly growing body of research on the gut–brain axis.
Here are some key points that help put the study into context:
- The gut and brain constantly communicate through biochemical signals.
- The microbiome influences inflammation, metabolism, and nervous system signaling.
- Disruptions in gut health have been linked to Parkinson’s disease progression.
- Many Parkinson’s patients experience gastrointestinal symptoms years before motor issues appear.
Because of these links, scientists increasingly believe that the gut might be one of the earliest sites affected in Parkinson’s disease. Using a gut-based therapy takes advantage of this connection and may even provide additional gastrointestinal benefits.
The Bigger Picture: Living Drugs for Chronic Diseases
What makes this research stand out is not only the potential Parkinson’s treatment, but the broader technological leap it represents. Bioengineered probiotics could one day be used to treat:
- Crohn’s disease
- Ulcerative colitis
- Mood disorders influenced by gut metabolites
- Other neurodegenerative diseases
- Metabolic disorders
This new therapy suggests a future where medicine isn’t just swallowed or injected—it’s colonized, living inside us, working continuously.
Of course, with any genetically modified organism intended for medical use, regulatory and safety challenges remain. Researchers will need to ensure:
- The bacteria don’t mutate in unintended ways
- They don’t disrupt the natural microbiome
- They don’t spread outside the body
- Their drug output remains stable and predictable
But if these hurdles are overcome, live biotherapeutics could become one of the most important medical innovations of the next decade.
Research Reference
Bioengineered gut bacterium synthesizing levodopa alleviates motor deficits in models of Parkinson’s disease
https://doi.org/10.1016/j.chom.2025.10.005