Novel Immunotherapy Shows Early Promise in Overcoming Resistance to Immune Checkpoint Treatments

A new Phase I clinical trial is offering cautious but genuine optimism for cancer patients who no longer respond to immune checkpoint inhibitors. Researchers at The University of Texas MD Anderson Cancer Center have reported encouraging early results for a novel monoclonal antibody called linavonkibart, which appears capable of helping tumors respond again to immunotherapy after resistance has developed. The findings were published in Nature Medicine and represent years of work focused on one of the most stubborn barriers in modern cancer treatment.
Why Immune Checkpoint Resistance Is a Big Problem
Immune checkpoint inhibitors, such as pembrolizumab, have transformed cancer care over the past decade. These drugs work by releasing the “brakes” on the immune system, allowing T cells to attack cancer more effectively. However, despite their success, a large proportion of patients either do not respond at all or eventually develop treatment resistance.
Research has increasingly pointed to a key biological culprit behind this resistance: transforming growth factor-beta 1 (TGFβ1). This protein helps tumors suppress immune responses and create an environment where immune cells struggle to function. Targeting TGFβ1 has long been considered a promising strategy—but until now, it has proven extremely difficult to do safely.
What Makes Linavonkibart Different
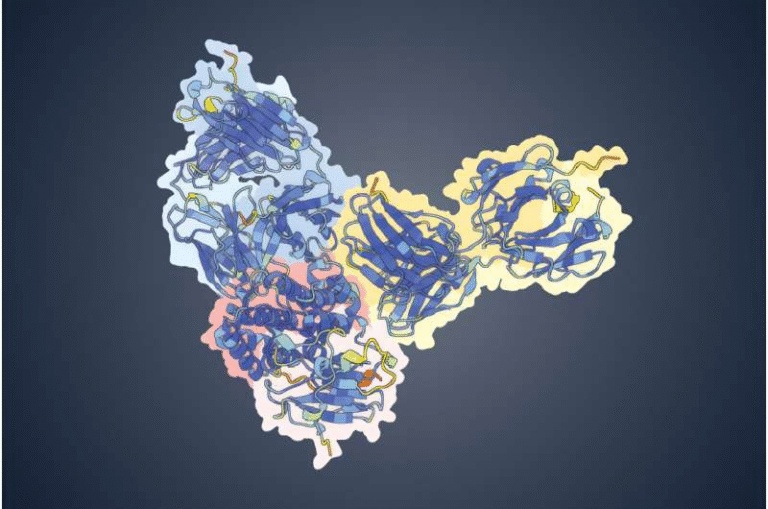
Linavonkibart is a first-in-class, fully human monoclonal antibody designed to selectively target only TGFβ1. This distinction matters. Earlier drugs aimed at the TGF-beta pathway blocked TGFβ1, TGFβ2, and TGFβ3 together, which led to severe side effects because TGFβ2 and TGFβ3 are essential for normal tissue maintenance and immune balance.
What sets linavonkibart apart is its precision. It binds to TGFβ1 in its inactive, or “off,” state and prevents it from becoming activated. By doing so, it neutralizes the immunosuppressive effects of TGFβ1 without interfering with the other TGF-beta proteins that the body needs to function normally.
Another important feature is that linavonkibart is fully human, meaning it is built entirely from structures naturally found in the human immune system. This reduces the risk of the body recognizing it as foreign and launching an immune attack against the drug itself. Early safety data from the trial support this design choice.
Inside the Phase I DRAGON Trial
The study, known as the DRAGON trial, was led by Timothy Yap, a professor of Investigational Cancer Therapeutics and vice president of clinical development at MD Anderson. The trial enrolled patients with advanced solid tumors who had already progressed on immune checkpoint therapy and had very limited treatment options remaining.
The trial was divided into three parts:
- Single-agent dose escalation arm: 19 patients, median age 66, with a median of four prior lines of therapy
- Combination dose escalation arm: 15 patients, median age 65, also with four prior lines of therapy, receiving linavonkibart plus pembrolizumab
- Combination dose expansion arm: 78 patients, median age 65, with three prior lines of therapy
These patients were considered heavily pretreated, and many had a prognosis measured in just a few months.
Safety Findings So Far
One of the most important goals of a Phase I trial is to evaluate safety, and in this area, linavonkibart performed well. The overall safety profile was manageable, both when used alone and in combination with pembrolizumab.
Notably:
- No grade four or grade five toxicities were observed in the dose escalation cohorts
- No dose-limiting toxicities occurred
- The side effects seen with the combination therapy were largely consistent with those already known for pembrolizumab
- Dermatologic reactions, such as rash, were the main additional side effect linked to linavonkibart
In the dose expansion cohort, rash was the most common grade three or higher adverse effect, and only four patients experienced any grade four side effects. These results suggest that selectively targeting TGFβ1 avoids the severe toxicity issues seen in earlier TGF-beta-blocking therapies.
Signs of Anti-Tumor Activity
While safety is the primary focus of early-phase trials, researchers also observed meaningful signals of clinical activity. Among the 78 patients in the combination dose expansion cohort—many of whom were progressing despite prior immune checkpoint therapy—multiple objective tumor responses were recorded.
The most striking results came from patients with advanced clear cell renal cell carcinoma, where a 20% objective response rate was observed. This is particularly notable given how heavily pretreated these patients were.
Responses were also seen in:
- Melanoma
- Head and neck squamous cell carcinoma
- Urothelial cancer
Importantly, these responses occurred in cancers that had already demonstrated resistance to PD-1 blockade, suggesting that linavonkibart may help re-sensitize tumors to immunotherapy.
Biomarkers and Patient Selection
Exploratory biomarker analyses revealed another promising angle: the potential to identify which patients are most likely to benefit from linavonkibart. In clear cell renal cell carcinoma, researchers uncovered early signals that specific biological markers could help enrich patient selection in future trials.
This approach could be crucial. Rather than treating all patients the same way, biomarker-guided strategies may allow clinicians to focus linavonkibart on those most likely to respond, improving outcomes while minimizing unnecessary exposure.
Why TGFβ1 Matters in Cancer Biology
To understand why these results are exciting, it helps to look more closely at TGFβ1’s role in cancer. In healthy tissues, TGFβ signaling helps regulate cell growth and immune balance. In cancer, however, TGFβ1 is often hijacked to:
- Suppress cytotoxic T-cell activity
- Promote immune exclusion from tumors
- Encourage tumor growth and metastasis
- Drive resistance to immunotherapy
By selectively blocking TGFβ1, linavonkibart aims to reverse immune suppression within the tumor microenvironment, allowing immune checkpoint inhibitors to work as intended.
What Comes Next for Linavonkibart
Researchers believe linavonkibart may be even more effective if used earlier in the course of treatment, before extensive resistance mechanisms take hold. Future studies are expected to explore this possibility, along with expanded trials in specific cancer types and refined biomarker strategies.
Early data from the DRAGON trial were also presented at the 2024 American Society of Clinical Oncology (ASCO) Annual Meeting, highlighting the broader oncology community’s interest in this approach.
A Cautious but Encouraging Step Forward
While linavonkibart is still in the early stages of development, the trial results suggest it could represent a meaningful advance in overcoming immune checkpoint resistance—one of the biggest challenges in cancer immunotherapy today. Larger and later-phase trials will be needed to confirm its effectiveness, but for now, the data offer a welcome sign that precision targeting of TGFβ1 may finally be within reach.
Research paper:
https://www.nature.com/articles/10.1038/s41591-025-04157-w