NU-9 Shows How Early Treatment Could Halt Alzheimer’s Disease Before Symptoms Begin
An experimental drug called NU-9, developed by researchers at Northwestern University, is offering a fresh and hopeful direction in Alzheimer’s disease research. In a new study published in Alzheimer’s & Dementia, scientists showed that NU-9 can stop some of the earliest biological changes linked to Alzheimer’s—before memory loss or other symptoms even begin—at least in animal models. The findings strengthen the idea that Alzheimer’s may need to be treated much earlier than current therapies allow.
Understanding Alzheimer’s as an Early-Beginning Disease
Alzheimer’s disease does not suddenly appear when memory problems start. Scientists now agree that the disease begins decades earlier, quietly progressing inside the brain. Long before symptoms become obvious, toxic proteins start accumulating, neurons become stressed, and immune cells in the brain shift into harmful states. By the time cognitive decline is noticeable, the underlying damage is already extensive, which helps explain why so many Alzheimer’s clinical trials have failed.
This new research focuses directly on that early, pre-symptomatic window, aiming to stop the disease before it gains momentum.
A Newly Identified Toxic Amyloid Culprit
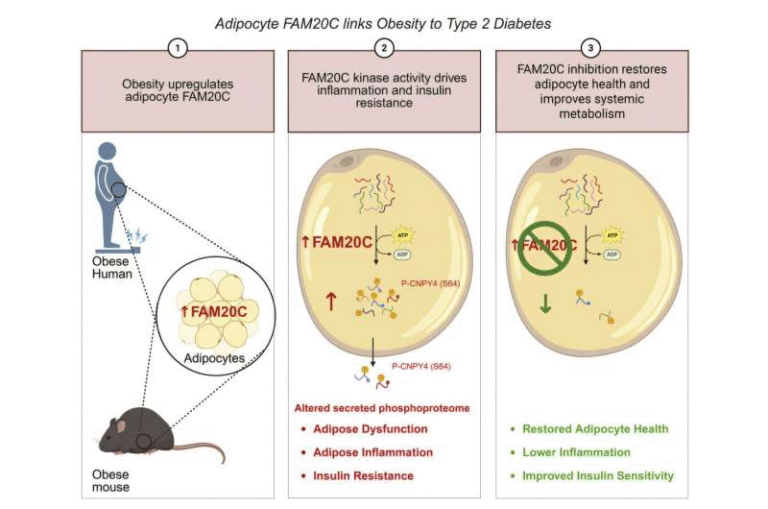
For years, researchers have known that amyloid beta oligomers—small clusters of amyloid beta protein—are more toxic than the larger plaques found later in Alzheimer’s disease. What this study uncovered is that not all amyloid beta oligomers behave the same way.
The Northwestern team identified a previously unknown and highly toxic subtype of amyloid beta oligomers that appears extremely early in disease development. This subtype, referred to as ACU193+, is detected using a specific antibody and shows up inside stressed neurons long before symptoms emerge.
Even more concerning, these toxic oligomers don’t stay confined to neurons. The researchers found that they migrate to nearby astrocytes, star-shaped glial cells that normally protect neurons and regulate inflammation. Once ACU193+ oligomers attach to astrocytes, they appear to trigger widespread inflammation, setting off a cascade of damage across the brain.
How NU-9 Works
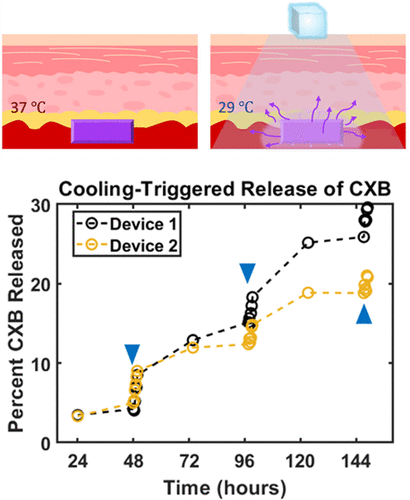
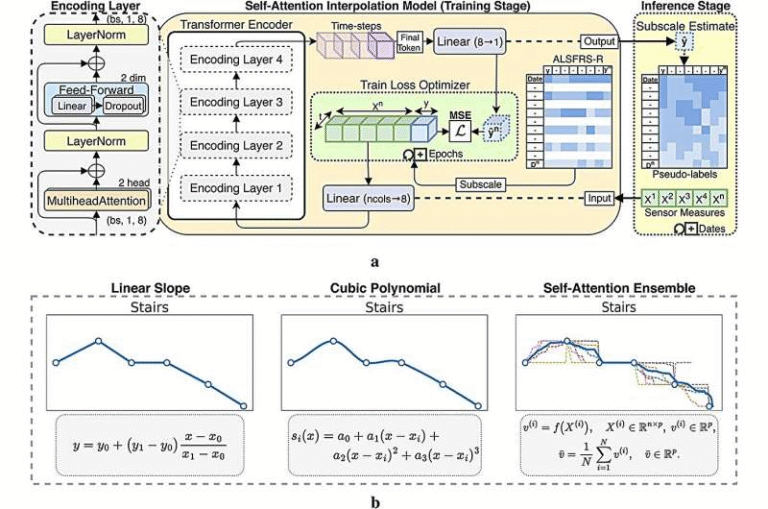
NU-9 is a small-molecule compound designed to restore the brain’s ability to clear toxic protein aggregates. In neurodegenerative diseases like Alzheimer’s and ALS, cells normally have systems to remove harmful proteins, but these systems become impaired over time. NU-9 appears to rescue that damaged pathway, allowing cells to clean themselves more effectively.
In this study, NU-9 dramatically reduced levels of the ACU193+ amyloid beta oligomer subtype. By doing so, it prevented astrocytes from entering a destructive, inflammatory state. This is a critical point, because reactive astrogliosis—an abnormal activation of astrocytes—is one of the earliest and most damaging inflammatory responses in Alzheimer’s disease.
Testing NU-9 Before Symptoms Appear
To evaluate NU-9’s potential as an early intervention, researchers used a pre-symptomatic mouse model of Alzheimer’s disease. These mice had not yet developed memory deficits or visible cognitive symptoms.
The animals received daily oral doses of NU-9 for 60 days. The results were striking. NU-9 significantly reduced early reactive astrogliosis across multiple regions of the brain. Toxic amyloid beta oligomers bound to astrocytes dropped sharply, and inflammation markers were greatly reduced.
The drug also lowered levels of abnormal TDP-43, a protein linked to cognitive impairment and found in several neurodegenerative diseases. Importantly, these improvements were not limited to one brain area—NU-9 produced a brain-wide anti-inflammatory effect.
Why Astrocytes Matter So Much
Astrocytes are often overlooked compared to neurons, but they play a central role in brain health. Under normal conditions, astrocytes support neurons, regulate chemical balance, and protect the brain from injury. However, when pushed into a reactive state, they become harmful.
Reactive astrocytes damage synapses, release inflammatory molecules, and accelerate neurodegeneration. Stopping astrocytes from becoming reactive may be one of the most powerful ways to slow or prevent Alzheimer’s progression, especially early in the disease. NU-9’s ability to block this process makes it particularly noteworthy.
Connections to ALS Research
NU-9 was not originally developed for Alzheimer’s disease. Conceived around 15 years ago, the compound emerged from long-term research aimed at clearing toxic protein buildup in neurodegenerative disorders.
By 2021, NU-9 showed strong effects in animal models of amyotrophic lateral sclerosis (ALS). It cleared toxic proteins such as SOD1 and TDP-43 and restored health to upper motor neurons. In 2024, NU-9 received U.S. FDA clearance to begin human clinical trials for ALS.
Given that toxic protein accumulation is a shared feature of ALS and Alzheimer’s, researchers began exploring whether NU-9 could work in Alzheimer’s disease as well. Earlier studies confirmed that NU-9 could clear toxic amyloid beta oligomers in lab-grown hippocampal brain cells. This new study extends those findings into living animal models.
A Preventive Approach to Alzheimer’s
One of the most intriguing ideas raised by the researchers is the possibility of using NU-9 as a preventive or prophylactic treatment. The concept is similar to how cholesterol-lowering drugs are used to prevent heart disease.
Having a biomarker for Alzheimer’s does not mean symptoms are imminent, but it could signal that early intervention is needed. As blood-based diagnostic tests for Alzheimer’s continue to improve, drugs like NU-9 could potentially be prescribed long before cognitive decline begins.
What Comes Next
The research team is now testing NU-9 in additional Alzheimer’s models, including a late-onset version that more closely resembles typical human aging. They also plan to follow treated animals for longer periods to see whether symptoms ever develop and how memory and neuron health are affected over time.
While NU-9 has not yet entered human trials for Alzheimer’s disease, the findings provide strong support for a new early-intervention strategy—one that targets toxic protein subtypes, suppresses inflammation, and protects brain cells before irreversible damage occurs.
Why This Study Stands Out
Many Alzheimer’s treatments focus on removing plaques after symptoms appear. This study takes a different and arguably more logical approach: stopping the disease before it becomes clinically visible. By identifying a hidden toxic driver and showing that it can be neutralized early, the NU-9 research opens a promising path forward.
The results do not mean Alzheimer’s has been cured, but they do suggest that timing may be just as important as the treatment itself.
Research paper:
https://alz-journals.onlinelibrary.wiley.com/doi/10.1002/alz.70968