Obese Patients Undergoing Shoulder Replacement Surgery Face No Increased Safety Risk, Large Study Shows

A new population-based study has delivered an important and somewhat surprising message for patients and clinicians: having a higher BMI does not increase safety risks for people undergoing elective shoulder replacement surgery. In fact, the study found that patients with obesity experienced equal or even better survival outcomes one year after surgery when compared to patients in the “healthy” BMI range. This research, led by Epaminondas Markos Valsamis from the University of Oxford and published in PLOS Medicine, adds weight to growing concerns about hospitals introducing BMI-based restrictions for joint replacement surgeries.
This article walks through the study’s findings in a clear and direct way, covering all specifics reported by the researchers. It also includes broader information about shoulder replacement surgery and how BMI has historically influenced surgical decision-making.
Credit: PLOS Medicine
What the Study Examined
The research team analyzed data from over 20,000 elective shoulder replacement surgeries performed across the United Kingdom and Denmark. In total, the dataset included:
- Approximately 15,320 surgeries from the UK
- Approximately 5,446 surgeries from Denmark
The goal was to understand whether body mass index (BMI) was linked to:
- Death within 90 days and 365 days after surgery
- Serious postoperative complications
- Risk of needing revision surgery (meaning the initial replacement failed or required correction)
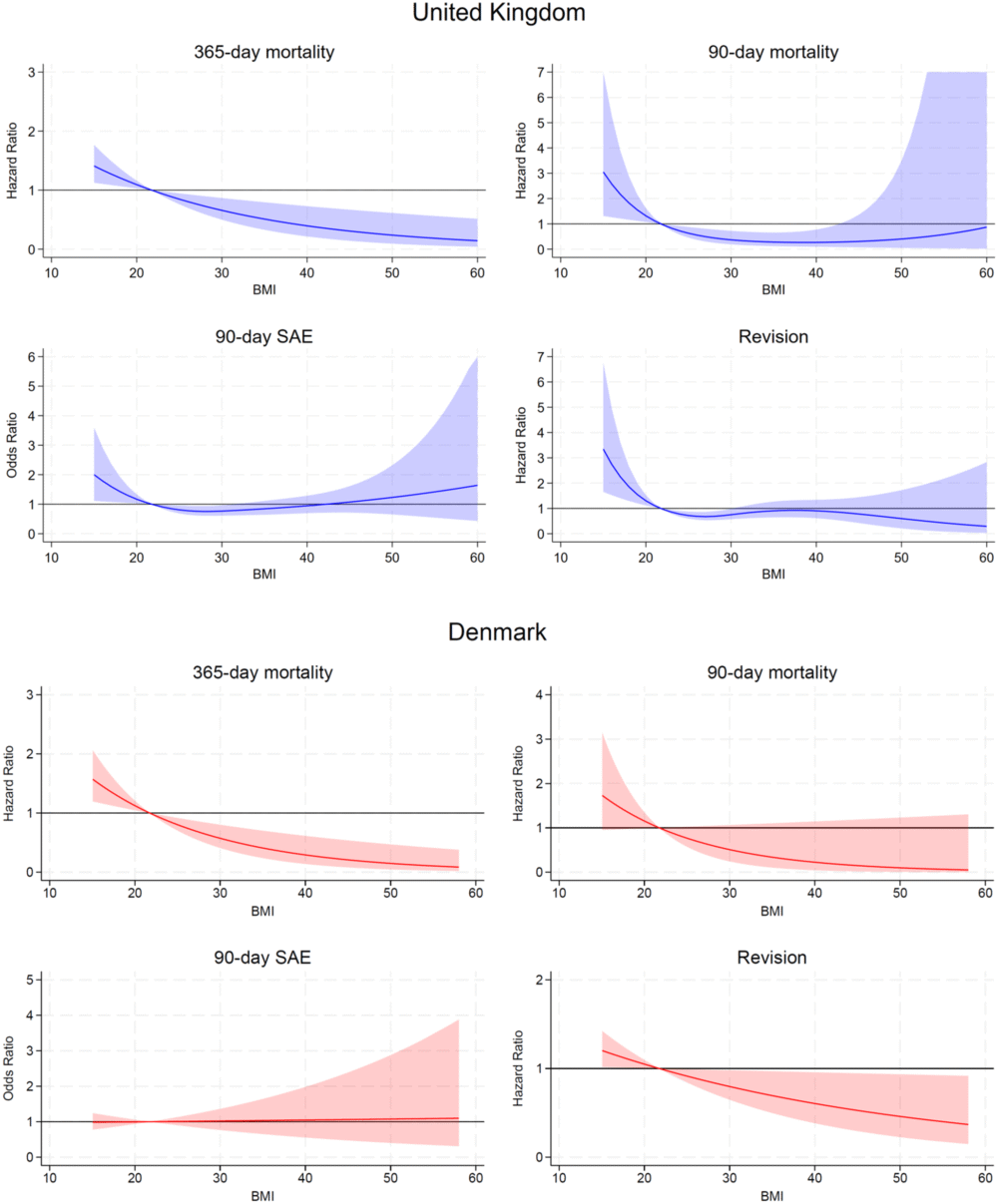
Researchers adjusted the data for several important factors, including age, sex, socioeconomic deprivation, surgical indication, and ASA score (a standardized measure of a patient’s overall health before surgery). A healthy reference BMI of 21.75 kg/m² was used for comparisons across outcomes.
Key Findings of the Study
A Lower Risk of Death for Patients With Obesity
One of the most striking outcomes was that patients with a BMI of 40 kg/m²—a level classified as obesity—had a 60% lower risk of death within one year after surgery compared to those with the reference BMI.
This directly challenges a long-held assumption that obesity automatically increases surgical risk. According to the study’s data, higher body weight did not translate to higher mortality or increased complications.
Higher Risks for Underweight Patients
In contrast, individuals who were underweight (BMI below 18.5 kg/m²) showed a slightly higher risk of death within a year of surgery. They also showed increased risk across multiple postoperative outcomes, including:
- Higher hazard ratios for 90-day mortality
- Increased risk of serious adverse events
- Elevated likelihood of needing revision surgery
However, it’s important to note that the underweight group was quite small:
- 131 patients in the UK dataset
- 70 patients in the Denmark dataset
Because of this smaller sample size, the researchers highlight that findings regarding underweight patients, while significant, should be interpreted with caution.
No Increased Complication Risks for Patients With Obesity
Beyond mortality, the study looked at several other factors. It found no increased risk for overweight or obese patients regarding:
- Serious adverse events within 90 days
- Need for revision surgery over several years
For all these outcomes, obesity simply did not appear to worsen the patient’s prognosis after shoulder replacement surgery.
What This Means for Access to Surgery
Despite the absence of any national guidelines recommending BMI cutoffs for joint replacements, many hospitals have adopted unofficial BMI limits, often denying or delaying surgery for people above a certain threshold.
The authors argue that this study does not support such restrictions. If anything, the data shows obese patients do just as well—or better—in key safety outcomes compared to other BMI groups.
This is especially important because:
- Shoulder replacements significantly improve quality of life, often restoring function and relieving severe chronic pain.
- Restricting surgery based on BMI alone may deny patients effective treatment without scientific justification.
- Using BMI as a rigid cutoff may reinforce stigma rather than reflect individual health status.
The senior author, Professor Jonathan Rees, emphasized that BMI thresholds should not determine access to joint replacement surgery. The findings reinforce the idea that healthcare decisions must be evidence-based, not based on assumptions.
Why Might Obesity Not Increase Risk Here?
Although the study does not attempt to explain why obese patients have lower mortality, several factors may play a role, and these are commonly discussed in orthopedic and anesthesia research:
1. Better Energy Reserves
People with higher BMI sometimes have greater physiological reserves, which can support recovery after major surgery.
2. Improved Detection and Management of Comorbidities
Obese patients often undergo more rigorous preoperative screening, which can lead to:
- Better detection of underlying issues
- More optimized management before surgery
3. The “Obesity Paradox”
This is a recognized phenomenon in medical literature where, in certain conditions, patients with obesity exhibit lower mortality. It remains a topic of ongoing investigation.
None of these explanations are definitive, but they do show that BMI alone is far from a complete measure of surgical risk.
Understanding Shoulder Replacement Surgery
To help readers better understand the context, here’s a concise look at what shoulder replacement surgery involves and why BMI discussions have become prominent.
What Is Shoulder Replacement?
A shoulder replacement—also called shoulder arthroplasty—is a procedure where damaged parts of the shoulder joint are replaced with artificial components, usually due to:
- Severe arthritis
- Major fractures
- Irreversible rotator cuff damage
Patients typically report:
- Significant pain relief
- Better mobility
- Improved daily function
Why Do Hospitals Use BMI Cutoffs?
Hospitals cite risks such as:
- Complications with anesthesia
- Higher infection rates
- Wound healing issues
However, the evidence for these concerns varies widely by surgery type. For shoulder replacement specifically, as this research shows, BMI does not correlate with increased risk for the key outcomes studied.
Why Low BMI Can Be Riskier
Being underweight is often associated with:
- Poor nutrition
- Low muscle mass
- Underlying chronic illness
All of these can negatively affect surgical outcomes and recovery.
Limitations of the Study
Every scientific study has limitations, and the authors acknowledge several:
- The underweight group was very small, which limits statistical power for that subgroup.
- There was a high proportion of missing BMI data in the national registries used.
- As an observational study, it cannot prove causation—only association.
- Unmeasured variables (smoking, physical activity, etc.) may also play a role.
Nonetheless, the consistency of the results across two different countries strengthens the reliability of the findings.
Final Thoughts
This study offers reassuring and important evidence: patients with obesity should not be denied shoulder replacement surgery based solely on BMI. With more than 20,000 patient cases analyzed, the research strongly supports a more inclusive and evidence-driven approach to surgical decision-making.
At the same time, it identifies underweight patients as a group that may need closer screening and support before and after surgery.
As hospitals increasingly consider BMI as a criterion for elective procedures, research like this is essential for ensuring fair access and accurate understanding of surgical risks.
Research Paper:
https://doi.org/10.1371/journal.pmed.1004786