Popular Diabetes and Weight-Loss Drugs Show Promise in Treating Alcohol and Drug Addiction

A new wave of research is revealing something fascinating about a class of medications many already know for managing diabetes and obesity — the GLP-1 receptor agonists (GLP-1RAs). Beyond helping people control blood sugar and lose weight, these drugs might also play a surprising role in reducing cravings for alcohol and other addictive substances.
A study published in the Journal of the Endocrine Society in October 2025, led by researchers from the National Institute on Drug Abuse (NIDA) and the National Institute on Alcohol Abuse and Alcoholism (NIAAA), offers strong early evidence that GLP-1 receptor agonists could become a new tool in treating alcohol and substance use disorders.
This isn’t just speculation — both animal studies and human trials are starting to back up the idea that GLP-1–based therapies may help reduce cravings, prevent relapse, and alter how the brain responds to addictive substances.
What Are GLP-1 Receptor Agonists?
GLP-1 receptor agonists, or GLP-1RAs, are a type of medication that mimic a natural hormone called glucagon-like peptide-1 (GLP-1). These drugs were originally designed for type 2 diabetes to help regulate blood sugar, and later became well-known for aiding in weight loss.
GLP-1 works by stimulating insulin release, slowing digestion, and reducing appetite. In simple terms, it helps people feel full faster and eat less. Drugs in this category include well-known names such as semaglutide (Ozempic, Wegovy), liraglutide (Saxenda, Victoza), and exenatide (Byetta).
But what’s even more interesting is that GLP-1 receptors aren’t just found in the gut and pancreas — they’re also present in the brain, particularly in regions that regulate reward, motivation, and decision-making. This is where addiction comes in.
Addiction and Its Challenges
Substance use disorders (SUDs) — including alcoholism, opioid addiction, and nicotine dependence — are among the most difficult conditions to treat. They’re characterized by loss of control, risky use, physical dependence, and social or behavioral problems.
According to the researchers, fewer than one in four people struggling with alcohol or drug addiction received any treatment in 2023. A mix of stigma, limited access to care, and lack of effective medications are major barriers.
Current treatments for alcohol or drug addiction, such as naltrexone, acamprosate, or buprenorphine, help some individuals but fail to address the full complexity of addiction. That’s why scientists are exploring new biological pathways — and GLP-1 receptor agonists are now at the forefront of that search.
How GLP-1 Drugs Might Affect Addiction
Researchers have discovered that GLP-1 affects the brain’s reward system, which plays a central role in both eating and addictive behavior. The same neural circuits involved in overeating — dopamine-driven pathways linked to pleasure and reward — are also involved in alcohol and drug cravings.
In essence, the brain mechanisms that make people overeat or crave sweets overlap with those that drive substance use. When GLP-1 receptor agonists activate certain parts of the brain, they appear to reduce dopamine release in response to rewarding substances like alcohol or opioids.
This doesn’t eliminate the desire completely, but it seems to dampen the craving and reduce compulsive behaviors. That’s why scientists are exploring whether GLP-1–based drugs can help people with addictions regain control — much like how they help with overeating and obesity.
What the Latest Research Shows
The October 2025 paper titled “GLP-1 Therapeutics and Their Emerging Role in Alcohol and Substance Use Disorders: An Endocrinology Primer” brings together findings from both preclinical (animal) and clinical (human) research.
Alcohol Use Disorder (AUD)
- In one study, the GLP-1 agonist exenatide — one of the first drugs in this class — showed no major change in alcohol consumption overall. However, in participants who also had obesity, exenatide did reduce alcohol intake.
- A newer study using semaglutide showed far more promising results. In people diagnosed with alcohol use disorder, low-dose semaglutide reduced alcohol self-administration in the lab, decreased the number of drinks per drinking day, and lowered craving levels.
Opioid Use Disorder
- Animal studies have shown that GLP-1 receptor agonists can reduce self-administration of opioids such as heroin, fentanyl, and oxycodone.
- These drugs also reduced relapse behavior in animal models — meaning the rodents were less likely to seek drugs again after a period of abstinence.
Tobacco Use Disorder
- In rodents, GLP-1 agonists reduced nicotine self-administration and relapse behavior.
- Early human studies suggest potential reductions in daily cigarette use and less weight gain after quitting — a common issue in smoking cessation.
The Science Behind It
The underlying mechanisms are complex, but researchers are zeroing in on a few key systems:
- Reward Pathways:
GLP-1 receptor activation in the brain’s ventral tegmental area (VTA) and nucleus accumbens — regions tied to pleasure and motivation — may reduce the rewarding effects of addictive substances. - Stress and Craving Regulation:
GLP-1 may influence the hypothalamic-pituitary-adrenal (HPA) axis, which plays a key role in stress responses and relapse triggers. - Cognitive Control:
These drugs might also affect prefrontal cortex activity, which governs self-control, impulse regulation, and decision-making — all of which are compromised in addiction. - Gut-Brain Connection:
Since GLP-1 is also active in the gut, part of its effect might be through gut-brain signaling, altering appetite, metabolism, and even mood in ways that influence addiction behaviors.
Real-World Data
Large-scale population studies are providing further support.
- A U.S. Veterans Affairs study involving nearly two million participants found that those taking GLP-1 drugs had a lower risk of developing substance use disorders, including alcohol, opioids, stimulants, and cannabis.
- Other studies observed that people on GLP-1 therapy had fewer hospitalizations for alcohol intoxication and lower recurrence rates for alcohol use disorder.
- Among people with opioid use disorder, GLP-1 therapy was linked to a significant reduction in overdose risk.
While these are observational findings (which show correlation, not causation), they add weight to the biological evidence from lab and clinical studies.
The First Human Trials
One of the most noteworthy clinical trials was published in JAMA Psychiatry in 2025. Researchers tested once-weekly low-dose semaglutide in 48 adults with alcohol use disorder.
Over nine weeks, participants who received semaglutide:
- Drank less alcohol in controlled lab settings.
- Reported lower craving scores throughout the study.
- Smoked fewer cigarettes (among those who smoked).
While small in scale, this was the first randomized, double-blind human trial showing that a GLP-1 receptor agonist could directly reduce alcohol consumption and craving. Larger studies are already being planned to confirm these results.
Why This Matters
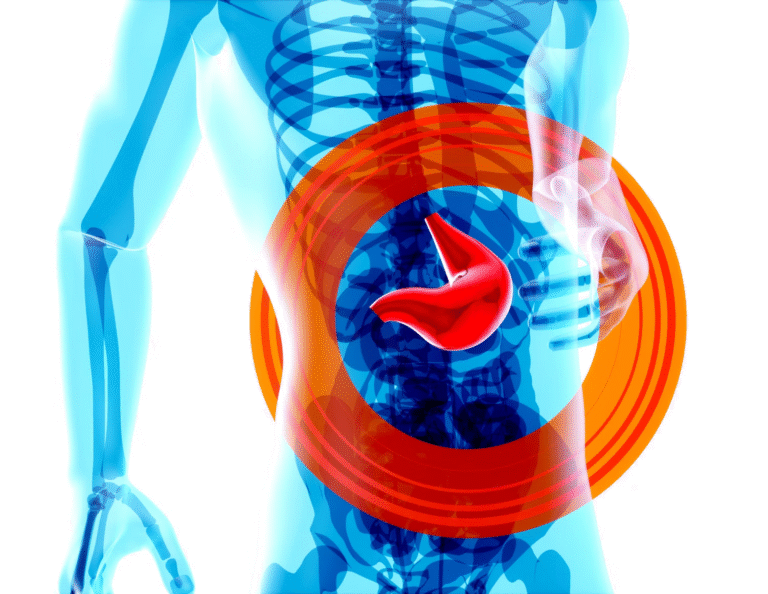
Addiction remains one of the leading causes of preventable illness and death worldwide. Alcohol alone contributes to millions of deaths annually, not just through liver disease, but also through accidents, violence, and chronic health conditions.
Despite the scale of the problem, medications for addiction are scarce and often ineffective for many patients. A new drug class that targets both biological and behavioral aspects of addiction — while also benefiting metabolic health — could transform the field.
What makes this discovery even more compelling is that GLP-1 drugs are already widely used, FDA-approved, and well-studied for safety in diabetes and obesity. Repurposing them for addiction could speed up access and reduce development costs.
Potential Limitations and Concerns
Of course, there are challenges ahead:
- Human trials are still limited — most studies so far are small or focused mainly on alcohol.
- Dosage and duration need optimization; what works for weight loss may not match what’s needed for addiction.
- GLP-1 drugs often cause nausea, vomiting, and gastrointestinal discomfort, especially at higher doses.
- People with substance use disorders often have liver problems, malnutrition, or other health issues, so safety and tolerability must be carefully studied.
- There’s also a concern about muscle loss and nutritional balance, which needs to be monitored in long-term treatment.
Despite these caveats, researchers remain cautiously optimistic. They emphasize that GLP-1–based therapy could complement, not replace, existing treatments like counseling, behavioral therapy, and existing pharmacological aids.
The Bigger Picture: Beyond Addiction
The discovery of GLP-1’s effects on the brain adds to a growing body of evidence showing how metabolic health and mental health are deeply connected. It suggests that the systems controlling hunger, mood, and reward are intertwined — meaning that treating one aspect (like appetite) can unexpectedly help another (like addiction).
It also opens up new research avenues into other compulsive behaviors, including binge eating, gambling, or even certain forms of impulsive spending. Early animal data hint that GLP-1 receptor pathways could influence many types of reward-seeking behaviors.
As more studies unfold, scientists hope to determine whether GLP-1 therapies can be personalized — for example, working better in people with both obesity and addiction, or those with specific genetic or neurological profiles.
Looking Ahead
The journey from diabetes drug to addiction treatment may still be in its early stages, but the path looks promising. Researchers from NIDA and NIAAA believe that larger, long-term trials will soon clarify exactly how effective these drugs are in reducing alcohol and drug use, and how best to use them alongside traditional addiction therapies.
For now, one thing is clear: GLP-1 receptor agonists are doing far more than helping people lose weight. They’re reshaping how scientists think about the biology of craving, reward, and self-control — and potentially offering hope for millions living with addiction.
Research Reference:
“GLP-1 Therapeutics and Their Emerging Role in Alcohol and Substance Use Disorders: An Endocrinology Primer” – Journal of the Endocrine Society, 9 October 2025