Scientists Show Alzheimer’s Disease Can Be Reversed in Animal Models With Full Brain Recovery

For more than a hundred years, Alzheimer’s disease (AD) has been viewed as a one-way condition. Once memory, cognition, and brain structure begin to decline, the assumption has been that the damage is permanent. Because of this belief, most Alzheimer’s research has focused on prevention or slowing disease progression, not on reversing damage that has already occurred.
A newly published study challenges that long-standing assumption in a major way. Researchers from University Hospitals, Case Western Reserve University, and the Louis Stokes Cleveland VA Medical Center report that Alzheimer’s-like disease can be reversed in animal models, leading to full neurological and cognitive recovery, even after the disease has reached an advanced stage.
The study was led by Dr. Kalyani Chaubey of the Pieper Laboratory and published in Cell Reports Medicine. While the findings are limited to animal models, the results represent a significant shift in how scientists might think about treating Alzheimer’s in the future.
Why Alzheimer’s Has Been Considered Irreversible
Alzheimer’s disease is characterized by widespread damage to the brain, including the buildup of amyloid plaques, abnormal tau protein tangles, neuroinflammation, loss of synaptic connections, and progressive neuron death. Once these processes begin, the brain’s ability to repair itself has been thought to be extremely limited.
Despite decades of research and billions of dollars invested, no Alzheimer’s drug has ever been tested in a clinical trial with the explicit goal of reversing disease and restoring lost function. Most therapies aim to delay decline, reduce symptoms, or slow the accumulation of pathological markers.
This new research directly challenges that mindset.
The Central Role of NAD+ in Brain Health
The study focuses on NAD+ (nicotinamide adenine dinucleotide), a molecule that plays a critical role in cellular energy metabolism, DNA repair, and cell survival. NAD+ is essential for normal brain function, but its levels naturally decline with age.
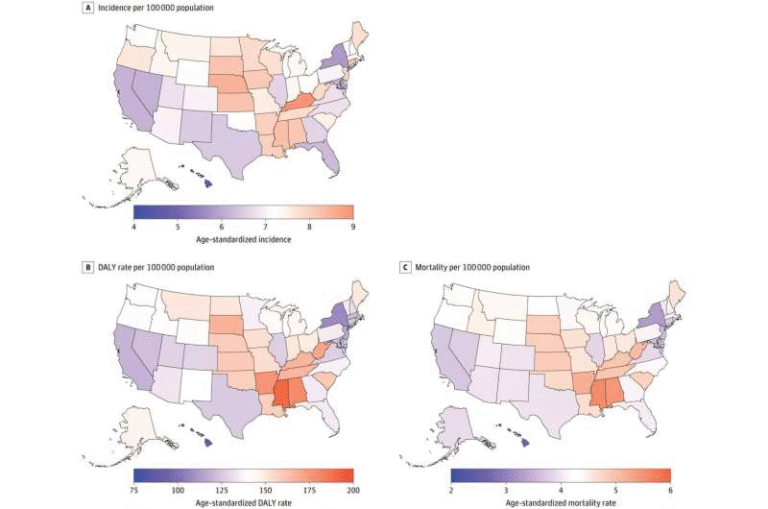
The researchers found that this decline is much more severe in the brains of people with Alzheimer’s disease, as well as in mouse models that mimic the condition. According to their findings, failure to maintain proper NAD+ balance is a major driver of Alzheimer’s pathology.
When NAD+ levels drop too low, brain cells lose the ability to perform essential tasks, repair damage, and survive long-term stress. Over time, this contributes to the widespread degeneration seen in Alzheimer’s.
Studying Alzheimer’s Using Two Distinct Mouse Models
Although Alzheimer’s is a uniquely human disease, researchers use genetically engineered mice to study its underlying biology. In this study, two very different mouse models were used:
- One model carried multiple human mutations related to amyloid processing
- The other model carried a human mutation in the tau protein
These two pathways—amyloid pathology and tau pathology—are among the earliest and most important events in Alzheimer’s disease. Both mouse models developed extensive brain damage similar to that seen in people with Alzheimer’s, including:
- Blood–brain barrier breakdown
- Axonal degeneration
- Chronic neuroinflammation
- Impaired hippocampal neurogenesis
- Reduced synaptic transmission
- Widespread oxidative damage
- Severe cognitive impairment
By using two genetically and biologically distinct models, the researchers strengthened their case that the observed effects were not limited to a single disease mechanism.
Restoring NAD+ Balance With a Targeted Drug
After confirming that NAD+ levels were sharply reduced in both human Alzheimer’s brains and mouse models, the team tested whether maintaining or restoring NAD+ balance could change disease outcomes.
To do this, they used a pharmacological compound called P7C3-A20, developed in the Pieper Laboratory. This compound had previously been shown to restore NAD+ balance and promote recovery after severe traumatic brain injury.
The approach was tested in two ways:
- Preventive treatment, where NAD+ balance was preserved before disease onset
- Delayed treatment, where NAD+ balance was restored after Alzheimer’s pathology was already advanced
The results were striking.
Full Cognitive and Pathological Recovery in Mice
In both mouse models, preserving NAD+ balance prevented the development of Alzheimer’s-like disease. Even more remarkable, delayed treatment in mice with advanced disease led to widespread recovery.
After treatment with P7C3-A20, researchers observed:
- Reversal of major pathological features caused by genetic mutations
- Restoration of normal brain structure and function
- Complete recovery of cognitive performance
In addition, blood levels of phosphorylated tau 217 (p-tau217)—a biomarker recently approved for clinical use in humans—returned to normal. This provided strong confirmation that disease reversal had occurred and highlighted a potential biomarker for future clinical trials.
Why This Matters for Alzheimer’s Research
Seeing the same recovery effect in two very different mouse models suggests that restoring brain energy balance could be a broadly effective strategy, rather than one limited to a specific genetic cause of Alzheimer’s.
The findings challenge the idea that Alzheimer’s damage is inevitably permanent. Under the right conditions, the brain appears capable of repairing itself and regaining lost function.
The researchers also identified specific proteins in human Alzheimer’s brains that may be linked to the ability to reverse disease, opening the door to additional therapeutic targets.
Important Safety Considerations Around NAD+
The researchers emphasized that their approach is not the same as taking over-the-counter NAD+ supplements. Some NAD+ precursors have been shown in animal studies to raise NAD+ levels too high, potentially increasing cancer risk.
The compound used in this study works differently. P7C3-A20 helps cells maintain proper NAD+ balance under stress, without pushing levels beyond normal physiological limits. This distinction is critical when considering future patient treatments.
Implications for Human Treatment and Next Steps
While the results are promising, the researchers stress that these findings are preclinical. Alzheimer’s in humans is far more complex than any animal model, and success in mice does not guarantee success in people.
The next step is carefully designed human clinical trials to determine whether restoring NAD+ balance can safely and effectively reverse Alzheimer’s disease in patients.
The technology behind this approach is already being commercialized through Glengary Brain Health, a Cleveland-based company co-founded by the study’s senior author.
Future research will focus on:
- Identifying which aspects of brain energy balance are most critical for recovery
- Exploring complementary therapeutic strategies
- Testing whether similar approaches could work in other age-related neurodegenerative diseases
A Shift in How Alzheimer’s Is Viewed
This study introduces a powerful new idea into Alzheimer’s research: recovery may be possible, not just prevention or delay. While human trials are still needed, the findings provide a scientifically grounded reason for optimism and a fresh direction for future therapies.
For a disease long defined by inevitability, that shift alone is significant.
Research Paper:
https://doi.org/10.1016/j.xcrm.2025.102535