Semaglutide Shows Strong Potential to Help Dialysis Patients Qualify for Kidney Transplants
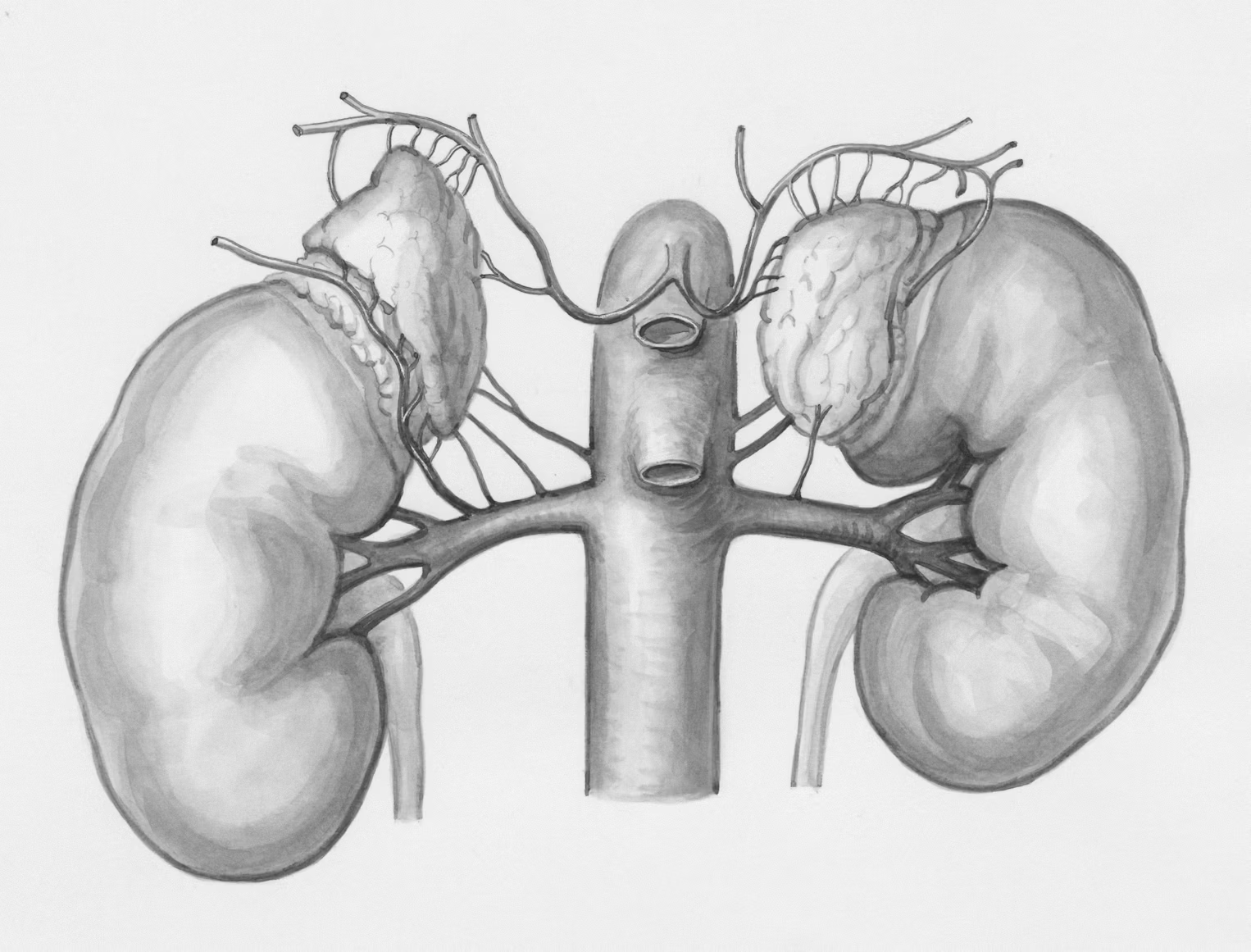
A new study from the Saint Louis University School of Medicine and SSM Health physicians offers a hopeful shift in transplant medicine, especially for dialysis patients struggling with obesity. The research focuses on Semaglutide, the active ingredient in well-known medications like Ozempic and Wegovy, and examines how effective it may be for patients with end-stage kidney disease who are often denied transplant eligibility due to a high body mass index (BMI).
The study, published in Clinical Transplantation, is one of the largest investigations to date evaluating Semaglutide specifically in dialysis patients. Traditionally, people on dialysis face enormous obstacles when they also live with obesity. Even when they meet all the medical criteria for a kidney transplant, a BMI above certain thresholds can result in automatic disqualification because of increased surgical risks and poorer post-transplant outcomes. This study directly tackles this long-standing barrier.
According to the findings, patients treated with Semaglutide for one year lost an average of 20.5 pounds, a meaningful amount for individuals who often struggle with weight loss due to metabolic complications of kidney failure, limited mobility, and treatment-related fatigue. Impressively, nearly 48.3% of patients who were previously ineligible for transplant due to weight were successfully activated on the kidney-transplant waitlist after losing enough weight. This is a notable milestone because waitlist activation is the crucial step that determines whether a patient even gets the chance to receive a donated kidney.
Another significant detail involves patients who were dependent on insulin for diabetes management. More than one-third of these individuals were able to stop insulin therapy entirely after incorporating Semaglutide into their treatment plan. This suggests weight loss wasn’t the only benefit—Semaglutide also offered metabolic improvements, which can dramatically improve quality of life.
The study reported that Semaglutide was generally well-tolerated. The most frequent side effects were gastrointestinal symptoms, a known issue with GLP-1 medications. About 16.7% of the patients discontinued the drug because of these side effects. The researchers also noted that patients on peritoneal dialysis appeared to experience GI symptoms more often compared to those receiving hemodialysis, though both groups were able to take the medication safely in most cases.
Another important element in the study is the emphasis on multidisciplinary care. At SSM Health Saint Louis University Hospital’s Comprehensive Metabolic Center, patients didn’t just receive Semaglutide. They also had access to nutrition counseling, exercise guidance, and regular follow-ups. This combined care approach is crucial because dialysis patients face unique weight-loss challenges—not only related to kidney disease itself but also because of fluid retention, inflammation, hormone changes, and medication interactions. Semaglutide alone is helpful, but it becomes even more effective when paired with professional lifestyle support.
Researchers involved in the study expressed optimism about how drugs like Semaglutide could transform transplant medicine. The rapid rise in popularity of GLP-1 medications such as Ozempic and Wegovy has already demonstrated their effectiveness in the general population. However, dialysis patients have historically been overlooked in weight-loss research. This study helps fill that gap, offering early evidence that the same medications helping millions lose weight might also open doors for people waiting for life-saving transplants.
Below, let’s explore some additional useful information related to Semaglutide, obesity, kidney disease, and the broader implications of this research.
Understanding Why BMI Matters in Kidney Transplants
Kidney transplant centers often use strict BMI cutoffs—typically ranging from 35 to 40—because patients with higher BMI values face greater risks such as wound complications, infections, and surgical difficulties. Some programs may even refuse to evaluate obese patients altogether.
For dialysis patients, this requirement is especially difficult. Dialysis can worsen fatigue and limit activity, making weight loss harder. Fluid retention can also artificially inflate weight, complicating BMI accuracy. That’s why medications that can help reduce body weight in a controlled, medically supervised way are becoming a major point of interest.
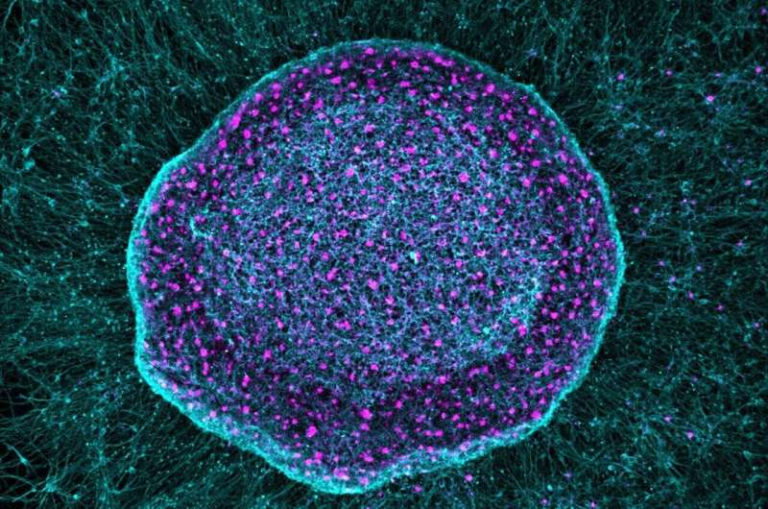
How Semaglutide Works in the Body
Semaglutide is a GLP-1 receptor agonist, a class of medications originally developed for type 2 diabetes. Its mechanisms include:
- Increasing feelings of fullness
- Slowing stomach emptying
- Supporting insulin production
- Reducing appetite
- Improving blood sugar control
These effects make it particularly helpful for patients dealing with obesity and diabetes—two conditions that frequently overlap with chronic kidney disease.
Semaglutide and Its Growing Role in Kidney Health
Beyond weight loss, Semaglutide has been investigated for broader kidney health benefits. Some recent studies (separate from the one discussed here) suggest that Semaglutide may reduce albuminuria, slow kidney disease progression, and lower cardiovascular risks. While this research is still early, it adds another layer of interest to the drug’s potential role in managing chronic kidney disease.
Unique Challenges for Dialysis Patients Trying to Lose Weight
Dialysis patients often face several barriers to traditional weight-loss strategies:
- Limited physical stamina
- Metabolic changes related to kidney failure
- Restricted diets that complicate calorie planning
- Medication side effects
- Chronic inflammation
This is why a medication offering clinically meaningful weight loss without major lifestyle changes is so valuable. For patients waiting for a transplant—a process that can take years—every pound lost increases their chances of being eligible for the surgery.
Why This Study Matters
This research represents a shift toward more inclusive and realistic approaches for transplant eligibility. Instead of expecting dialysis patients to lose large amounts of weight on their own, clinicians now have a powerful tool to help them meet life-saving requirements.
If Semaglutide continues to show positive outcomes in larger or longer-term studies, transplant centers may begin integrating GLP-1 medications into standard pre-transplant protocols. That could potentially increase the number of transplant-eligible patients nationwide.
The study also highlights the importance of treating obesity as a medical condition rather than a personal failure. For dialysis patients, obesity is not only common—it is often a downstream result of the disease itself. Addressing it through modern, evidence-based treatments can significantly improve access to transplantation.
Looking Ahead
As GLP-1 medications become more widely used, many experts believe transplant medicine is entering a new era. More research will be needed to understand long-term outcomes, especially for patients who remain on Semaglutide after receiving their kidney transplant. But for now, the findings provide a strong signal that medications like Ozempic may help bridge one of the biggest gaps in kidney-transplant accessibility.
Research Reference
Bridging the Gap to Waitlist Activation: Semaglutide’s Weight Loss Efficacy and Safety in Patients With Obesity on Dialysis Seeking Kidney Transplantation
https://doi.org/10.1111/ctr.70344