Study Reveals a Promising New Therapeutic Target for Treating Glaucoma

Researchers have uncovered an important new clue in the fight against glaucoma by identifying a specific group of cells in the eye’s drainage system that show early signs of failure. This discovery points toward a potential new therapeutic strategy that could help slow or even prevent the progression of this vision-threatening disease.
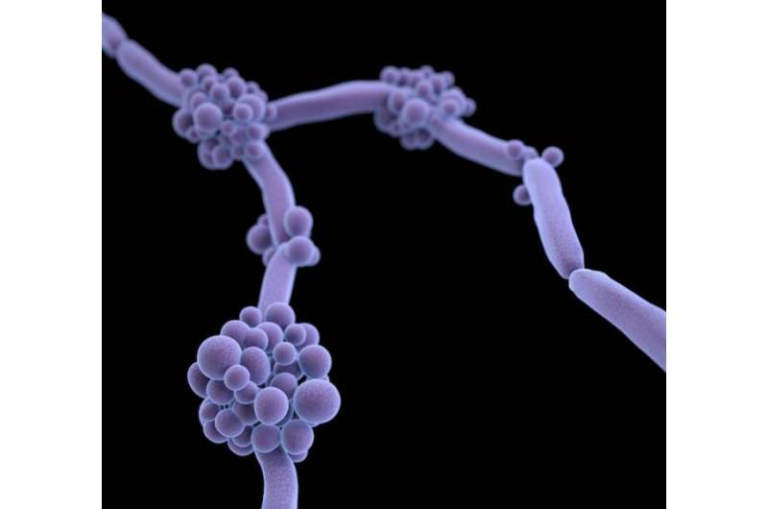
The study, published in the journal eLife, focuses on the trabecular meshwork, a critical but often overlooked tissue responsible for regulating fluid outflow from the eye. When this system fails, eye pressure can rise, increasing the risk of optic nerve damage. By mapping this tissue at the single-cell level, scientists were able to pinpoint which cells are most vulnerable in glaucoma and why they matter.
Why glaucoma remains such a serious global problem
Glaucoma is not a single disease but a group of eye disorders that damage the optic nerve, the structure responsible for sending visual information from the eye to the brain. Once this damage occurs, it is irreversible. As of 2020, glaucoma affected around 80 million people worldwide, making it one of the leading causes of permanent blindness.
One of the biggest risk factors for glaucoma is elevated intraocular pressure. In many cases, this pressure increases because fluid inside the eye cannot drain efficiently. That drainage process depends heavily on the trabecular meshwork, a sponge-like tissue located in the limbal region, where the clear cornea meets the white sclera.
Despite its importance, scientists have long known surprisingly little about the cellular makeup of the trabecular meshwork and how individual cell types respond to stress and disease.
Building a detailed cellular map of the trabecular meshwork
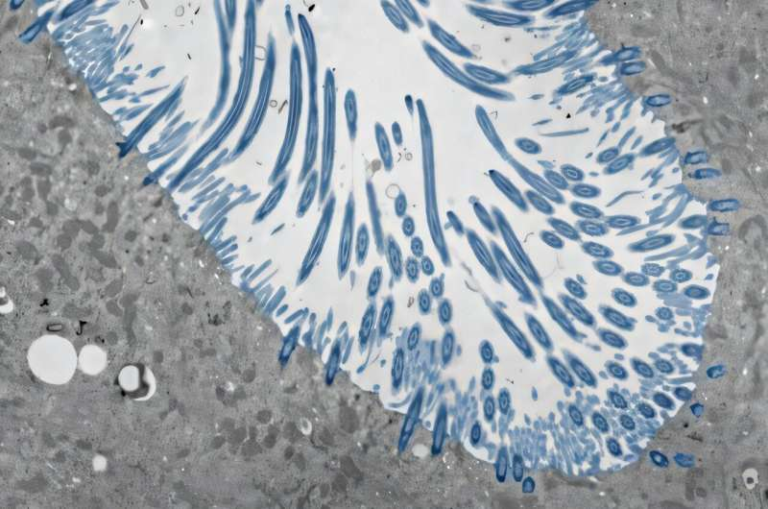
To address this gap, the research team used single-cell RNA sequencing, a powerful technique that reveals which genes are active in individual cells. By applying this method, they analyzed nearly 18,000 cells taken from the limbal region of two healthy mouse strains.
This detailed analysis revealed six major cell types in the region. Among them were three distinct subtypes of trabecular meshwork cells, which the researchers labeled TM1, TM2, and TM3.
The identities of these cell types were carefully validated using multiple approaches. These included comparisons across independent datasets, confirmation in different laboratories, and imaging techniques such as immunofluorescence, which highlights specific proteins, and in situ hybridization, which shows where certain genes are active within tissue.
Each of the three TM subtypes showed a unique molecular signature and occupied specific locations within the trabecular meshwork, suggesting that they play different roles in maintaining eye health.
What makes TM1, TM2, and TM3 different?
The TM1 cells were rich in genes related to extracellular matrix production. This finding suggests that TM1 cells help maintain the structural integrity of the trabecular meshwork, ensuring that the tissue can withstand constant fluid flow.
The TM2 cells expressed genes involved in cell signaling and phagocytosis, a process that allows cells to engulf and remove debris. This points to a possible role in immune surveillance and cleanup within the drainage system.
The most intriguing group, however, was TM3. These cells showed high expression of genes linked to mitochondrial function and cell contractility, meaning they are metabolically active and likely involved in controlling fluid resistance. TM3 cells also stood out because they strongly expressed Lmx1b, a gene already known to be associated with glaucoma in both mice and humans.
How genetic glaucoma affects specific cells
To understand how these cell types behave under disease conditions, the researchers turned to a genetic mouse model of glaucoma. These mice carry a dominant mutation in the Lmx1b gene, which closely mimics inherited forms of glaucoma.
All three trabecular meshwork cell types were still present in these mutant mice. However, TM3 cells were disproportionately affected. They showed clear signs of mitochondrial dysfunction, including reduced activity in oxidative phosphorylation, the main process cells use to generate energy.
In addition, TM3 cells displayed lower expression of genes involved in protein quality control, which helps cells manage damaged or misfolded proteins. Together, these changes suggest that TM3 cells experience early metabolic stress, making them less capable of regulating fluid outflow properly.
This selective vulnerability helps explain how relatively subtle genetic changes can eventually lead to increased eye pressure and glaucoma progression.
Exploring mitochondrial support as a treatment strategy
One of the most practical and exciting aspects of the study involved testing a potential intervention. The researchers treated some of the glaucoma-model mice with nicotinamide, a form of vitamin B3 known to support cellular metabolism and mitochondrial health.
The results were encouraging. Mice that received nicotinamide showed lower intraocular pressure and fewer of the structural changes typically associated with glaucoma progression. In contrast, untreated mice continued to show worsening signs of disease.
These findings suggest that supporting the metabolic health of TM3 cells may help preserve trabecular meshwork function and protect against glaucoma-related damage. While more work is needed to understand exactly how vitamin B3 exerts its effects, the study highlights metabolism as a promising new therapeutic angle.
What this means for future glaucoma research
This work provides the most comprehensive characterization of trabecular meshwork cell diversity to date. By identifying which cells are most vulnerable and why, the study opens the door to more targeted therapies that go beyond simply lowering eye pressure.
Importantly, the findings raise questions about whether similar TM3-like cells exist in the human eye and whether metabolic treatments such as nicotinamide could offer long-term protection in clinical settings. Answering these questions will require further research, including human tissue studies and controlled clinical trials.
Extra context: why mitochondria matter in eye diseases
Mitochondria are often described as the power plants of the cell, and tissues with high energy demands are especially sensitive to mitochondrial dysfunction. The eye, particularly structures involved in pressure regulation and neural signaling, relies heavily on efficient energy production.
In recent years, mitochondrial impairment has been implicated in several eye diseases, including glaucoma, optic neuropathies, and age-related degeneration. This study adds to growing evidence that protecting cellular metabolism may be just as important as managing mechanical factors like eye pressure.
A step toward more precise glaucoma treatments
Rather than treating glaucoma as a uniform condition, this research supports a more cell-specific and mechanism-based approach. By targeting the cells that fail first and understanding the biological processes behind that failure, future therapies may become more effective and less invasive.
While nicotinamide is not yet a proven treatment for human glaucoma, the concept of metabolic protection offers a fresh direction in a field that has long relied on pressure-lowering drugs and surgery.
Research paper: https://elifesciences.org/articles/107161