Why the Brain’s Memory Circuit Collapses First in Alzheimer’s

One of the enduring mysteries of Alzheimer’s disease is why memory circuits in the brain collapse so early, long before other regions show signs of damage. New research from Virginia Tech’s Fralin Biomedical Research Institute at VTC sheds light on this question, pointing directly to mitochondrial stress and calcium overload as potential culprits.
The Vulnerable Entorhinal Cortex
The study focuses on the entorhinal cortex, a critical region for memory, spatial navigation, and the brain’s internal mapping system.
This part of the brain is one of the first to deteriorate in Alzheimer’s, leading to the early memory issues associated with the disease. Researchers are probing why this particular area is so fragile compared to other regions.
Funding for this work comes from the Commonwealth of Virginia’s Alzheimer’s and Related Diseases Research Award Fund (ARDRAF), which supports projects aimed at uncovering the mechanisms of Alzheimer’s and related dementias.
The Research Team and Their Expertise
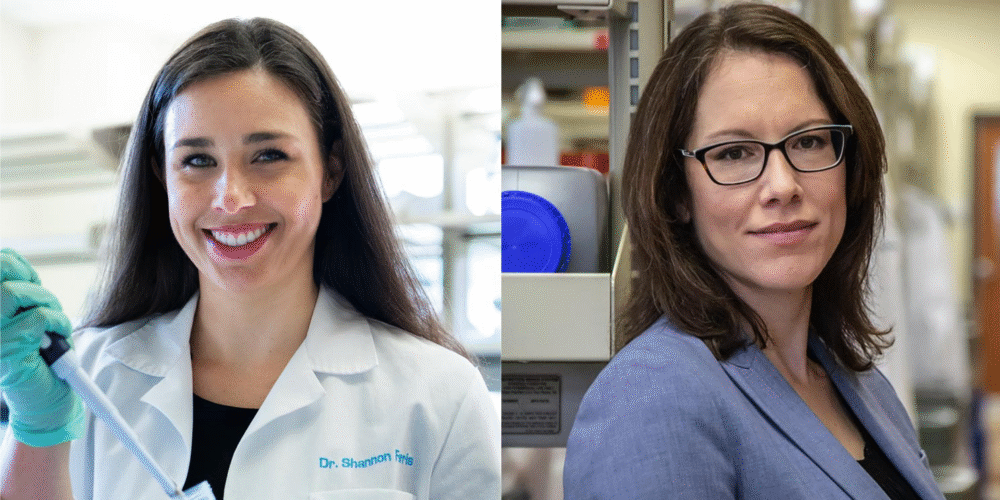
The project is led by Sharon Swanger and Shannon Farris, both scientists at Virginia Tech’s Fralin Biomedical Research Institute and faculty members in the Department of Biomedical Sciences and Pathobiology at the Virginia-Maryland College of Veterinary Medicine.
- Swanger studies how brain cells communicate across synapses in circuits that are known to be vulnerable to disease.
- Farris investigates how memory-related brain circuits function at the molecular level, with a focus on mitochondria.
Their combined expertise creates a direct way to explore how synaptic communication and mitochondrial function interact in Alzheimer’s disease, a connection often overlooked in the field.
Why Mitochondria Matter
Mitochondria, often called the power plants of the cell, provide the energy neurons need for essential tasks like synaptic transmission. In Alzheimer’s disease, mitochondria become dysfunctional, leaving neurons underpowered and more likely to fail.
The researchers are examining whether mitochondria in the entorhinal cortex and related circuits are particularly vulnerable because of calcium overload. Calcium is a vital chemical for neuronal communication, but too much of it can push mitochondria into stress and eventually trigger cellular breakdown.
Watching Early Failure in Real Time
One of the striking findings so far is that synapses in these circuits show unusually strong calcium signals in nearby mitochondria. These signals are so large that they can be seen clearly under a light microscope—a rare observation in neuroscience research.
Such strong calcium activity could be a direct reason why the entorhinal cortex fails first in Alzheimer’s. By identifying and watching these early disruptions, researchers now have a real-time model for studying the earliest stages of the disease.
The Experiment in Detail
To test their hypothesis, the team is using brain tissue from healthy mice and mice that carry Alzheimer’s-like pathology. By comparing the two groups, they aim to uncover exactly how mitochondrial function differs between healthy and disease-affected circuits.
Credit: Virginia Tech
The central goal is to spot early warning signs of stress or failure in the entorhinal cortex–hippocampus circuit, the pathway most closely linked to memory loss in Alzheimer’s. Identifying these early breakdowns could lead to diagnostic markers or therapeutic strategies aimed at preserving mitochondrial function before irreversible damage occurs.
Support for State-Level Research
The researchers also stress the importance of state-level funding. Programs like ARDRAF give scientists the ability to take risks on projects that might open new directions in understanding complex diseases. While national funding is often focused on larger-scale efforts, targeted state support allows labs to dig deeper into specific, unanswered questions.
Broader Scientific Context
This work fits into a growing body of evidence that mitochondrial dysfunction and calcium dysregulation are major drivers of Alzheimer’s progression. Studies from other institutions highlight that circuits demanding high energy and precise calcium balance—like those in the entorhinal cortex and hippocampus—are more prone to early degeneration.
The Virginia Tech project is unique because it provides a direct experimental model where researchers can observe the interaction between calcium overload and mitochondrial stress in live tissue. This level of detail could help identify intervention points for future therapies.
Looking Ahead
By focusing on the earliest breakdowns in memory circuits, Swanger and Farris are addressing a critical gap in Alzheimer’s research. Most current treatments target symptoms that appear much later, but preventing or slowing the initial collapse of the entorhinal cortex could change the trajectory of the disease altogether.
The findings also underscore the potential for therapies aimed at regulating calcium signaling or strengthening mitochondrial resilience. If successful, such approaches might help preserve memory function in the earliest and most vulnerable stages of Alzheimer’s disease.
TL;DR
Virginia Tech researchers are studying why the entorhinal cortex collapses early in Alzheimer’s. Their work shows mitochondria in memory circuits get overloaded with calcium, causing stress and failure. Using mouse models, they’re tracking these early breakdowns to guide future therapies.
Research link: ScienceDirect – Mitochondrial dysfunction in Alzheimer’s disease