Year-Round RSV Immunization Could Reduce Seasonal Outbreaks Across Urban and Rural Communities
A growing body of research is reshaping how scientists and public health experts think about respiratory syncytial virus (RSV), one of the most common and dangerous respiratory infections affecting infants and young children. A new study published in Science Advances suggests that offering RSV immunization year-round, rather than limiting access to a seasonal window, could significantly reduce the risk of large outbreaks across the United States—no matter whether communities are urban or rural.
RSV is a leading cause of lower respiratory tract infections in infants and young children. In the United States alone, it accounts for around 80,000 hospitalizations each year among children under the age of five, with infants under one year old facing the highest risk of severe illness. While preventive tools such as maternal vaccines and antibody treatments for infants have become available in recent years, they are typically offered on a seasonal basis, timed to what is assumed to be the RSV season. This new research challenges the idea that RSV has a single, predictable season everywhere.
How RSV Behaves Differently in Cities and Rural Areas
The study closely examined how RSV spreads in areas with different population densities, focusing on differences between urban and rural communities. Researchers analyzed hospitalization records for young children and identified distinct patterns in how RSV outbreaks unfold depending on where people live.
In urban areas, RSV outbreaks tend to last longer and occur at a lower but more sustained intensity. Importantly, a higher proportion of hospitalized cases involve infants under one year of age. This matters because younger infants have less developed respiratory systems, making them more vulnerable to severe complications.
In contrast, rural areas experience RSV outbreaks that are shorter and sharper, often described as “spikier.” While these outbreaks may be intense, they do not persist as long as those seen in cities.
One of the key drivers behind these differences appears to be patterns of interpersonal contact. Cities naturally involve more frequent and sustained interactions between people. Although infants themselves are not navigating public transportation or crowded spaces, urban families are more likely to rely on daycare settings, where many young children come into close contact. These environments provide ideal conditions for RSV transmission among the age group most susceptible to severe disease.
Learning From Other Respiratory Viruses
Interestingly, the researchers noted that RSV’s urban–rural behavior mirrors patterns seen with influenza. Flu viruses tend to persist year-round in densely populated areas because people consistently interact in shared spaces. However, RSV differs from influenza in one critical way: it is primarily transmitted among very young children, not adults.
This makes the findings especially important. While adults drive much of flu transmission, RSV spreads largely through infant and toddler contact networks, particularly in daycare and early childcare settings. This distinction helps explain why cities see more sustained RSV activity, even though babies themselves are not moving through society the same way adults do.
Modeling the Impact of Immunization Strategies
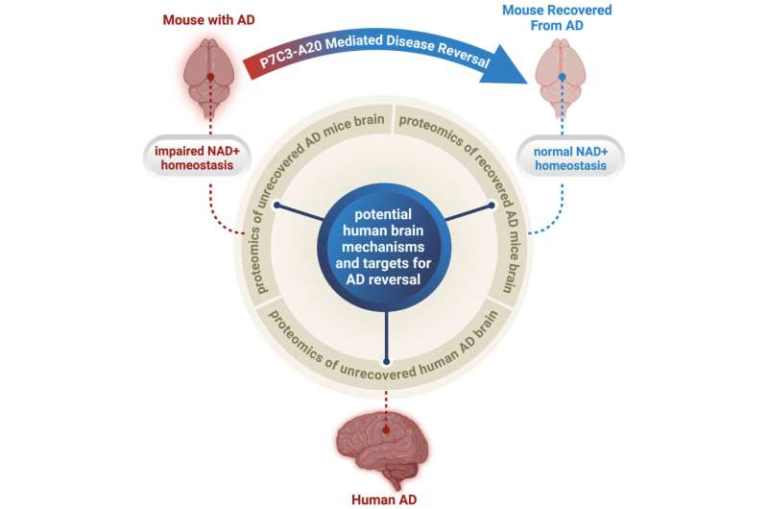
To better understand how immunization policies could influence RSV outbreaks, the research team built mathematical models that incorporated real-world data on population density, contact patterns, and hospitalization rates. These models allowed the researchers to simulate what would happen under different immunization strategies.
Two main approaches were tested: seasonal immunization, which mirrors current practice, and year-round immunization access.
The models confirmed that any increase in immunization coverage reduces RSV hospitalizations, which is an encouraging result. However, they also revealed a potential downside to strictly seasonal programs. When protection is only offered during a defined window, infection rates can rise outside that window, particularly during unexpected off-season periods. In some scenarios, this could even lead to summer RSV outbreaks, something that seasonal strategies are not designed to handle.
By contrast, year-round access to RSV immunization consistently reduced the risk of large outbreaks. This approach smoothed out transmission patterns and minimized sharp spikes in infections, regardless of whether communities were urban or rural.
Why RSV Seasonality Is Hard to Pin Down
One of the most important takeaways from the study is that RSV timing varies widely across the United States. Previous research has shown that northern states often experience large RSV epidemics every two years, while southern states and tropical regions may see annual or even near year-round circulation.
More recently, the COVID-19 pandemic disrupted normal RSV patterns even further. As masking and social distancing measures were relaxed, unexpected RSV surges occurred in 2023 and 2024, confirming earlier predictions made by the same research group. These shifts highlight a key problem with seasonal immunization strategies: they rely on the assumption that RSV follows a predictable calendar.
According to the study’s findings, that assumption no longer holds true. RSV does not behave like a virus with a single, fixed season, making it difficult to define an “optimal” vaccination window that works everywhere.
Implications for Public Health Policy
The researchers argue that a more flexible, risk-averse approach would be to provide RSV immunization whenever individuals are eligible, rather than tying access to a specific season. This would mean offering vaccination to pregnant women within the recommended gestational window and protective antibody treatments to infants in the appropriate age group at any time of year.
Such an approach could be especially beneficial in protecting infants during their first RSV exposure, which often occurs at the youngest and most vulnerable ages in urban environments. By reducing the likelihood of delayed or missed protection, year-round access could lower hospitalizations and ease strain on healthcare systems.
A Closer Look at RSV and Prevention Tools
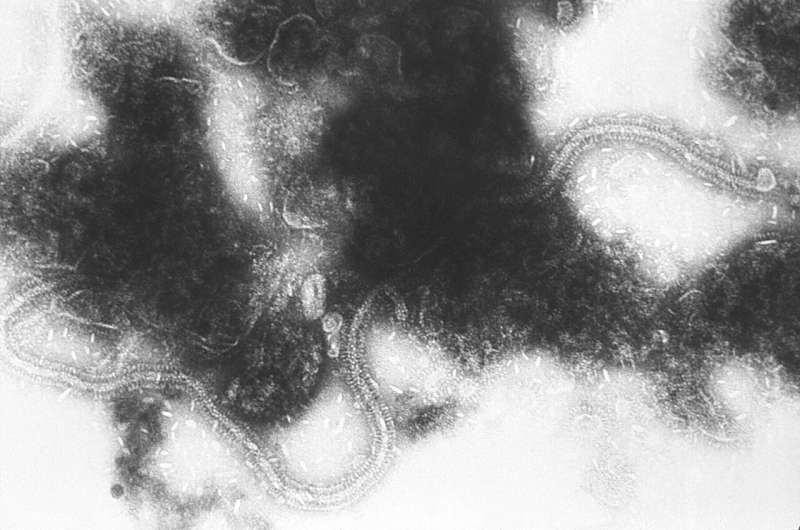
RSV spreads through respiratory droplets and contaminated surfaces, and it can survive for hours on hands and objects. Symptoms range from mild cold-like illness to severe bronchiolitis and pneumonia, particularly in infants, premature babies, and children with underlying health conditions.
In recent years, prevention options have expanded. A maternal RSV vaccine can protect newborns through transferred antibodies, while monoclonal antibody treatments offer direct protection to infants during their highest-risk months. These tools have already shown success in reducing severe disease, but their full potential may only be realized with more adaptable delivery strategies.
Looking Ahead
This study adds to a growing recognition that one-size-fits-all seasonal vaccination policies may not work for RSV. By accounting for differences in population density, contact patterns, and regional timing, year-round immunization access could offer a more robust defense against a virus that continues to surprise public health systems.
As RSV prevention continues to evolve, the findings provide strong evidence that flexibility and accessibility may be just as important as the vaccines themselves.
Research paper:
https://www.science.org/doi/10.1126/sciadv.ady5457