MIT’s New Nanoparticle Therapy Helps T Cells Destroy Ovarian Tumors While Avoiding Dangerous Side Effects
Researchers at the Massachusetts Institute of Technology (MIT) have developed a new nanoparticle-based treatment that could transform how doctors approach ovarian cancer, one of the most difficult cancers to treat using current immunotherapy methods. The study, published in Nature Materials in 2025, demonstrates how specially engineered nanoparticles carrying interleukin-12 (IL-12) can supercharge the body’s immune response to ovarian tumors — without the severe side effects that have plagued IL-12 treatments in the past.
Why Ovarian Cancer Is So Difficult to Treat
Ovarian cancer remains one of the deadliest cancers among women because it’s often diagnosed late and tends to spread rapidly throughout the peritoneal cavity — the space around the abdomen that includes organs like the intestines, pancreas, and liver. Standard treatment usually involves surgery followed by chemotherapy. While this can shrink tumors, the disease often comes back, sometimes in more aggressive forms.
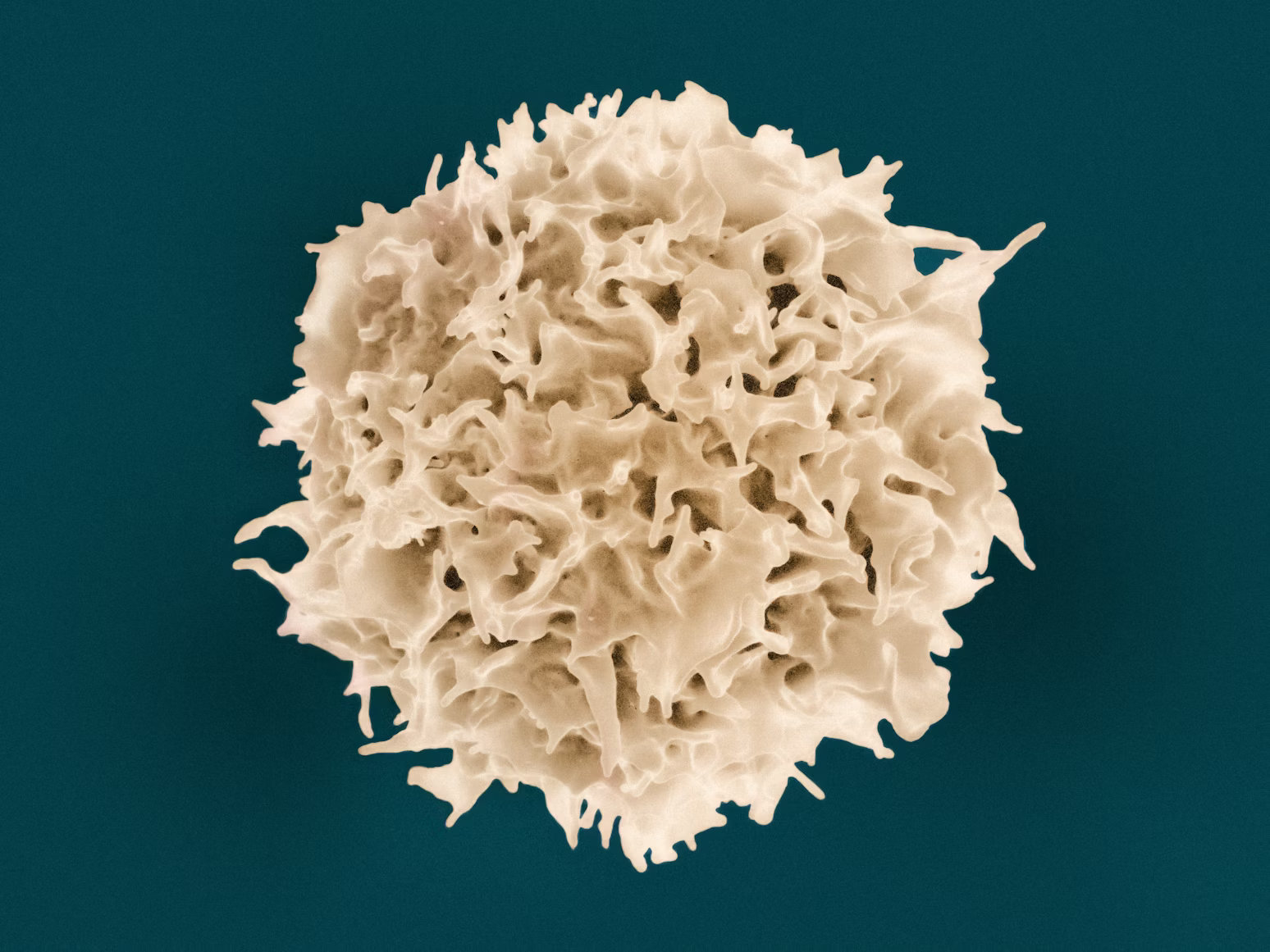
Immunotherapy, which harnesses the immune system to fight cancer, has shown major success in some cancers like melanoma and lung cancer. These treatments, known as checkpoint inhibitors, work by “taking the brakes off” the immune system. However, ovarian tumors create a microenvironment filled with immune-suppressing proteins, which prevent T cells — the immune system’s main tumor killers — from doing their job.
As a result, even when doctors “release the brakes” using checkpoint inhibitors, there’s no real acceleration — the immune system simply doesn’t get the signal to attack. Researchers refer to this as a “cold” tumor environment. MIT’s team decided to find a way to “hit the gas.”
The Role of IL-12 and Why It’s Risky
Interleukin-12 (IL-12) is a powerful immune-stimulating molecule known to activate T cells and natural killer (NK) cells, helping them recognize and destroy cancer cells. It essentially acts like a megaphone for the immune system, amplifying its response.
However, there’s a huge problem: delivering IL-12 systemically — through injections into the bloodstream — causes widespread inflammation throughout the body. Patients in earlier trials suffered severe side effects such as high fevers, fatigue, gastrointestinal distress, liver toxicity, and in some cases, even life-threatening cytokine release syndrome.
Because of these risks, IL-12 therapy was largely abandoned in clinical settings. The MIT researchers wanted to change that by finding a safer way to deliver IL-12 directly to the tumor site, avoiding the rest of the body.
How MIT’s Nanoparticles Work
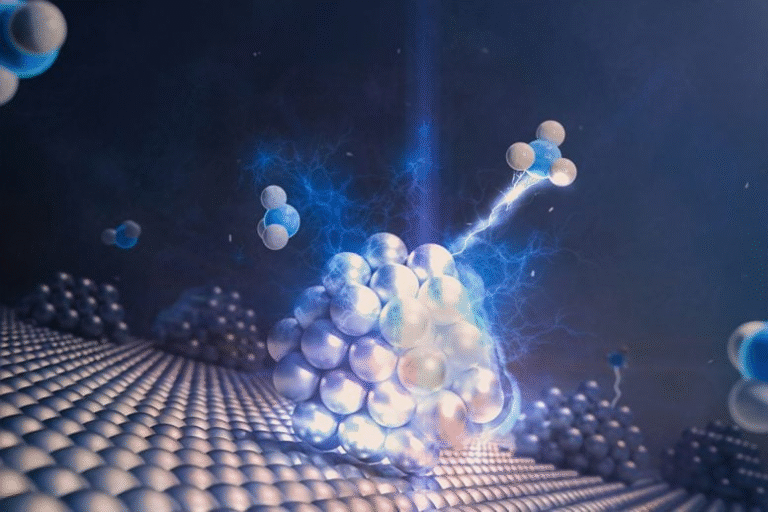
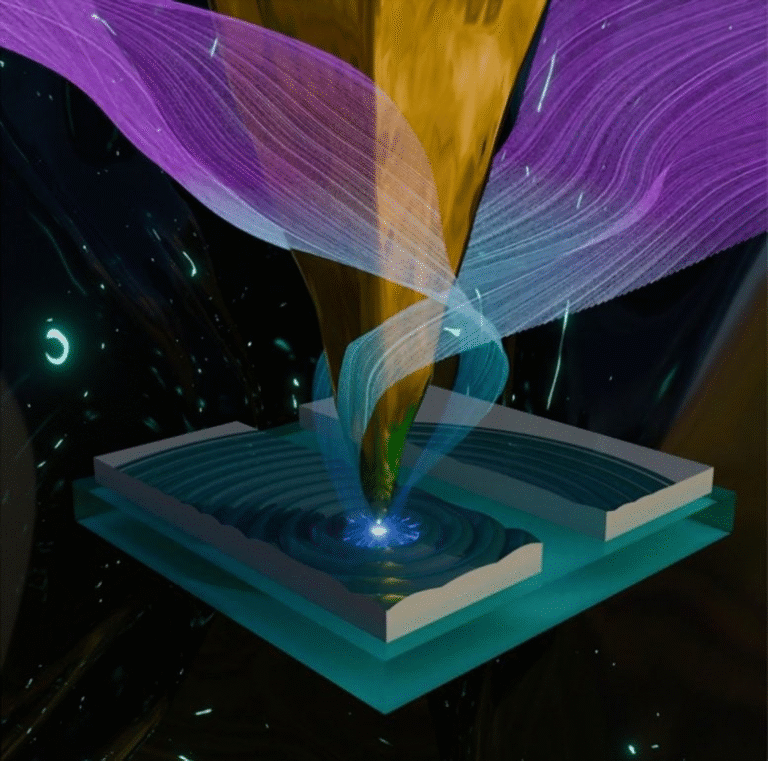
The new treatment uses liposomal nanoparticles — tiny fat-based droplets that act as miniature delivery capsules. Each nanoparticle carries IL-12 molecules attached to its surface using a maleimide chemical linker, which keeps the cytokine firmly tethered to the particle. This linker is more stable than older versions used in previous designs that released IL-12 too quickly.
To make sure these particles find the right target, the scientists coated them with a polymer layer of poly-L-glutamate (PLE). This coating helps the nanoparticles bind specifically to ovarian tumor cells in the peritoneal cavity. Once they reach the tumor, they slowly release IL-12 over about a week, allowing the immune system to be stimulated locally — right where it’s needed.
This slow, controlled release is crucial. Earlier versions of IL-12 nanoparticles dumped their payload too quickly, limiting how long immune cells stayed active. By improving the release rate, the team achieved a stronger and longer-lasting T cell response without triggering systemic inflammation.
The Results: Tumors Disappearing in Mice
The researchers tested this system on mice with metastatic ovarian cancer, a model that mimics how the disease spreads throughout the abdomen. In these mice, tumors were found not only in the ovaries but also across organs like the liver and pancreas, and even in the lungs.
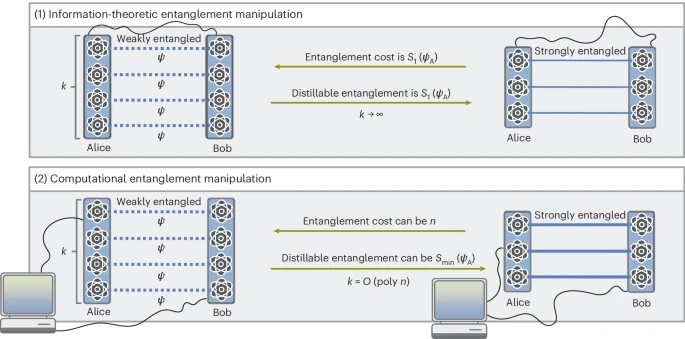
When treated with the IL-12 nanoparticles alone, about 30% of the mice were completely cured of their tumors. Importantly, when the nanoparticles were combined with checkpoint inhibitors — drugs that free up the immune system to attack cancer — the results were dramatic: over 80% of the mice were completely tumor-free.
Even more remarkable, when scientists later reintroduced ovarian cancer cells into the same mice several months later, their immune systems remembered the tumor’s proteins and wiped out the new cancer cells automatically. This demonstrated that the treatment created long-term immune memory, something rarely seen in ovarian cancer therapies.
Reduced Side Effects and Stronger Immune Response
Blood tests showed that the nanoparticle system limited IL-12 exposure in the bloodstream, which helped avoid the toxic side effects normally caused by this cytokine. The treatment led to a significant increase in T cells inside the tumors, especially CD8+ T cells, which are the main cancer-killing subtype.
The immune environment inside the tumor also changed in other ways. Immune-suppressing regulatory T cells (Tregs) decreased, while macrophages — a type of immune cell — shifted from tumor-supporting M2 types to inflammatory, tumor-fighting M1 types. This created a microenvironment where cancer cells were no longer protected from the immune system.
Why This Research Matters
This new nanoparticle system could open the door to a powerful combination strategy: pairing local immune activation with systemic checkpoint blockade. In simpler terms, it could finally make “cold” tumors like ovarian cancer respond to immunotherapy.
If successful in humans, this approach might also help treat other cancers that have been resistant to immunotherapy, such as pancreatic, colorectal, or prostate cancers, which share similar immunosuppressive features.
The Science Behind the Design
At a molecular level, the nanoparticles are built as liposomes — spherical structures made from phospholipid bilayers. The IL-12 is chemically anchored to these lipids, and then the surface is coated using a layer-by-layer (LbL) technique. This involves alternating layers of positively and negatively charged polymers, which helps fine-tune both stability and release rate.
The final product is a highly stable particle that travels through the peritoneal cavity, sticks to tumor surfaces, and gradually leaks IL-12 into the surrounding tissue. The nearby T cells then become highly activated, multiply, and attack the tumor cells directly.
When combined with checkpoint inhibitors like anti–PD-1 or anti–CTLA-4 antibodies, these reinvigorated T cells can destroy even stubborn tumor cells that previously resisted immune attack.
The Bigger Picture: What’s Next for This Research
Although these results are extremely promising, they are still preclinical, meaning they’ve only been tested in mice so far. Human trials are the next step, but the researchers emphasize that several hurdles remain, such as verifying safety, scaling up production, and ensuring the nanoparticles behave the same way in human patients.
The team, led by Paula Hammond (MIT Institute Professor and Vice Provost for Faculty) and Darrell Irvine (Professor of Immunology and Microbiology at Scripps Research Institute), is already collaborating with MIT’s Deshpande Center for Technological Innovation to create a startup aimed at developing the technology for clinical use.
They’ve also developed new manufacturing methods that make it easier to produce these nanoparticles in large batches, which is essential for any potential human trials.
While there’s still a long way to go before patients can benefit from this breakthrough, this work represents a major step toward making immunotherapy work for ovarian cancer, one of the toughest cancers to treat.
Understanding Nanoparticles and Immunotherapy
For readers less familiar with the science, nanoparticles are typically 1 to 100 nanometers wide — about a thousand times smaller than a human hair. Their small size and customizable chemistry allow them to carry drugs, proteins, or genetic material directly to specific tissues. They’ve been used in COVID-19 mRNA vaccines and are increasingly being explored for cancer therapy.
Meanwhile, immunotherapy focuses on using the body’s own defenses rather than chemical agents to fight disease. The most well-known immunotherapy drugs are checkpoint inhibitors, which target proteins like PD-1, PD-L1, and CTLA-4 that normally act as safety switches to prevent the immune system from attacking healthy cells.
In cancers like ovarian cancer, these switches are often overactive, keeping the immune system “off.” Combining checkpoint inhibitors with IL-12 nanoparticles effectively releases the brakes and hits the gas at the same time — a one-two punch that could be key to lasting remission.
Research Paper Reference: IL-12-releasing nanoparticles for effective immunotherapy of metastatic ovarian cancer – Nature Materials (2025)