Nanoparticle Blueprints Reveal How Tiny Carriers Could Lead to Smarter Medicines

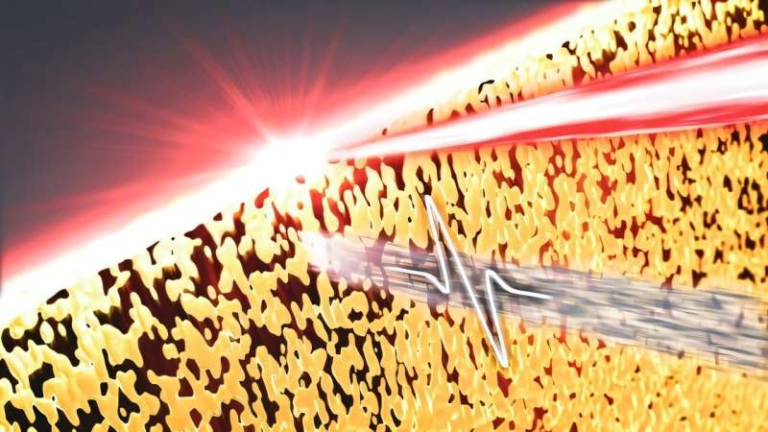
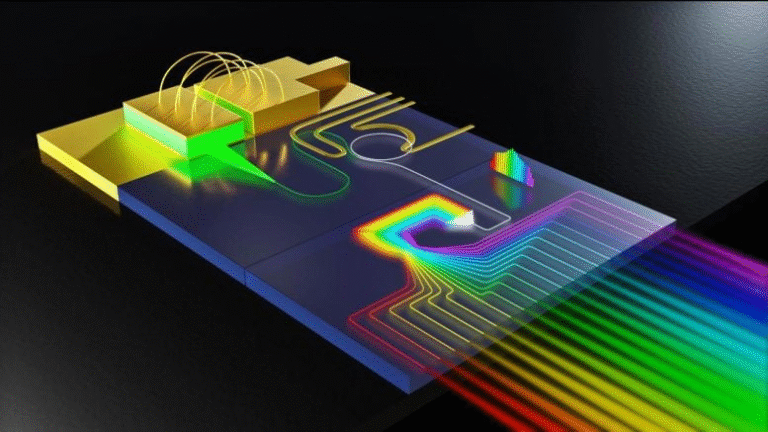
Lipid nanoparticles, or LNPs, are the invisible workhorses behind many of today’s medical breakthroughs—from mRNA vaccines and gene therapies to cancer treatments. These microscopic spheres (or so we thought) act as delivery vehicles, carrying therapeutic materials like RNA and drugs into the body’s cells.
For years, scientists assumed that all LNPs were more or less the same: small, spherical packages that worked efficiently regardless of the therapy. But a new study from the University of Pennsylvania, in collaboration with Brookhaven National Laboratory and Waters Corporation, just turned that assumption on its head. Published in Nature Biotechnology (October 2025), the research reveals that LNPs are not neat little balls at all. Instead, they vary in shape, structure, and internal organization—differences that profoundly influence how well they deliver medicine.
This discovery could pave the way for designing “smarter medicines”, where the structure of each nanoparticle is intentionally tuned for a specific therapeutic target—be it the liver, immune cells, or tumors.
Breaking Down the Myth of the Perfect Sphere
Until recently, most studies treated LNPs like identical spheres—imagine a fleet of uniform trucks rolling off the same assembly line. But the team led by Michael J. Mitchell (Penn Engineering) and Kushol Gupta (Penn’s Perelman School of Medicine) found something far more complex.
LNPs, it turns out, are shaped more like jelly beans than marbles—irregular, diverse, and full of hidden variation even within a single formulation. These differences aren’t just cosmetic. They change how the particles behave inside the body—how much therapeutic material they release, where they deliver it, and how efficiently they work.
This finding challenges a fundamental assumption of nanoparticle medicine. It suggests that there is no universal “best” LNP. Instead, each therapy might need its own custom-designed particle, much like choosing between a pickup truck, a delivery van, or a freight truck depending on the job.
How the Researchers Saw What Others Couldn’t
LNPs are extremely small—thousands could fit across a single human hair. Because of that, visualizing their shape and structure is difficult. Previous studies often relied on just one analytical method, sometimes freezing the particles or tagging them with fluorescent dyes. Both techniques risked altering their shape and obscuring the natural variation among them.
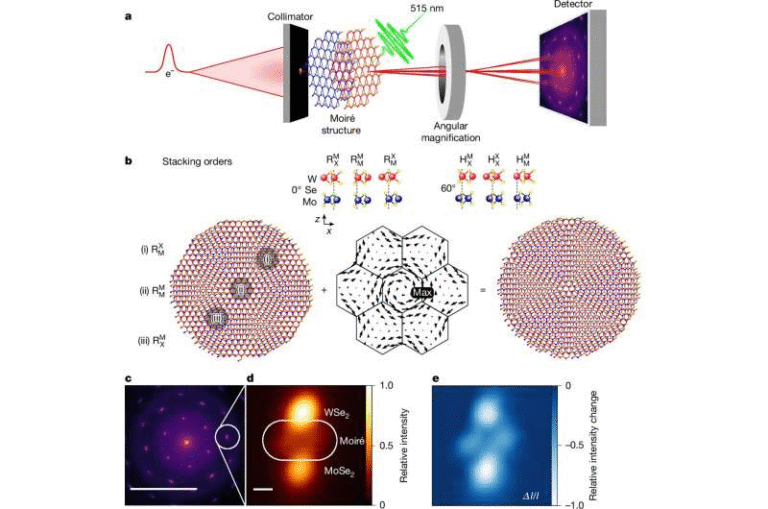
The new study took a more comprehensive approach, combining three advanced biophysical techniques that allowed scientists to study the nanoparticles intact and in solution, revealing their true structure.
The Three Techniques
- Sedimentation Velocity Analytical Ultracentrifugation (SV-AUC):
This technique spins LNPs at extremely high speeds to separate them by density. It helps determine how much RNA or other therapeutic cargo each particle contains and reveals variations across the population. - Field-Flow Fractionation Coupled with Multi-Angle Light Scattering (FFF-MALS):
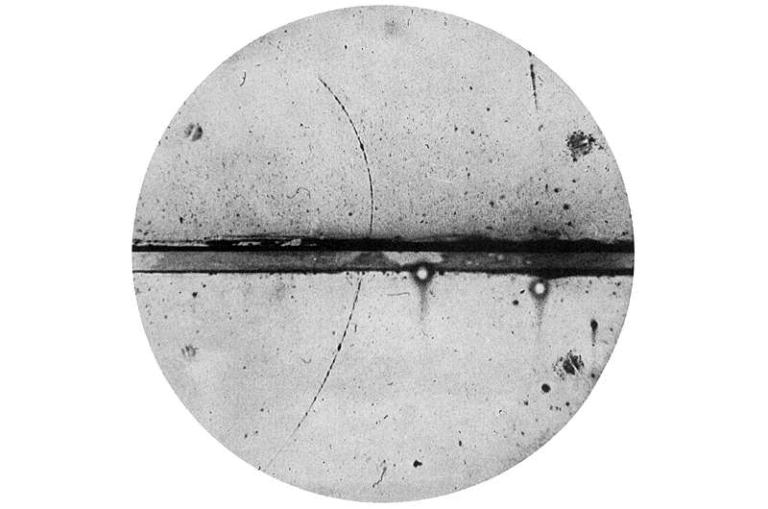
This method gently separates nanoparticles by size and measures how the nucleic acid cargo is distributed among them. - Size-Exclusion Chromatography In-Line with Synchrotron Small-Angle X-Ray Scattering (SEC-SAXS):
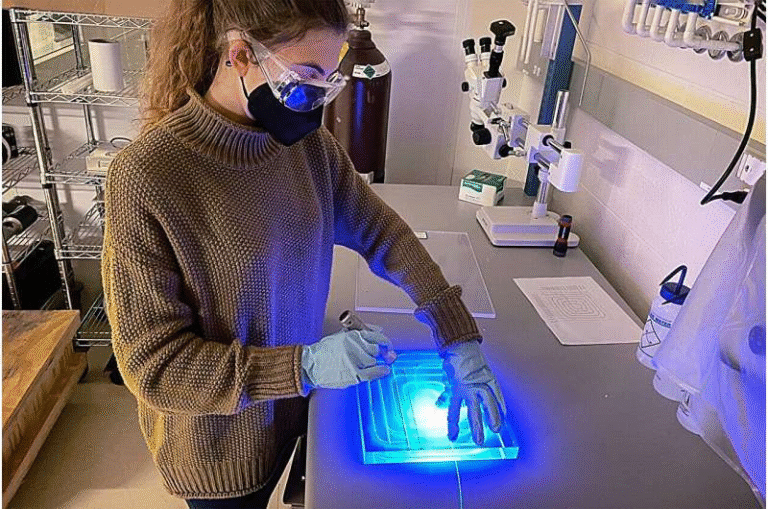
This is where things get really high-tech. Conducted at Brookhaven National Laboratory’s National Synchrotron Light Source II, the SEC-SAXS method bombarded nanoparticles with powerful X-rays to reveal their internal architecture without damaging them.
By comparing results across these techniques, the researchers could confirm that what they were seeing wasn’t an artifact of the method—it was the real, complex structure of LNPs.
What They Discovered
The study examined four “gold-standard” LNP formulations, including those used in COVID-19 vaccines and in Onpattro, an FDA-approved therapy for a rare genetic disease.
The results were striking:
- LNPs differ in size, shape, and internal structure even when produced from the same recipe.
- Their structure depends heavily on the lipid composition (the types of lipids used) and the manufacturing process (how ingredients are mixed).
- Different LNP structures correlated with differences in how effectively they delivered genetic material into cells.
In short, structure matters. Some shapes delivered RNA payloads more efficiently to immune cells, while others performed better in animal models targeting other tissues.
Testing How Structure Affects Function
To test whether these structural variations actually changed how LNPs work, the researchers evaluated their performance in a series of biological experiments.
They used multiple models—human T cells, cancer cells, and animal models—to measure how much therapeutic material each type of particle could deliver. They found that specific structural traits were tied to better outcomes, such as more efficient delivery or more successful “unloading” of cargo once inside the cell.
Interestingly, the “best” LNPs weren’t always the ones that looked most uniform or consistent. In some cases, particles with more irregular shapes or mixed internal structures performed better in specific biological contexts.
Why the Manufacturing Method Matters
Another major insight came from comparing how LNPs were made. Two methods were tested:
- Microfluidic mixing, where ingredients are forced through small tubes for highly controlled assembly.
- Manual pipette mixing, where ingredients are mixed by hand at the bench.
The assumption has long been that microfluidics produces better, more consistent nanoparticles—and it usually does. But in certain cases, hand-mixed particles performed better, delivering more cargo or achieving stronger biological responses.
This shows that how you make the nanoparticles can be just as important as what they’re made of. Think of it like baking cookies: the same ingredients can yield different results depending on how you mix them.
The Role of Collaboration
This study wouldn’t have been possible without combining the strengths of different institutions.
- The University of Pennsylvania team contributed expertise in nanoparticle biology and formulation.
- Brookhaven National Laboratory provided access to the synchrotron facility that made high-resolution X-ray scattering possible.
- Waters Corporation, through its Wyatt Technology division, helped measure particle size and composition using advanced light-scattering tools.
By pooling their resources, these groups managed to visualize nanoparticles at a level of detail that had never been achieved before. The collaboration highlights how breakthroughs often come from the intersection of academia, industry, and government research facilities.
Why This Matters for Medicine
Understanding the link between structure and function in nanoparticles could transform how future therapies are designed. Rather than relying on trial and error, scientists can now start designing LNPs intentionally for specific tasks.
For example:
- LNPs designed to target immune cells could be optimized for vaccine delivery.
- Those meant to reach the liver might have different shapes or lipid compositions.
- Cancer therapies might use particles with unique internal structures for better tumor penetration.
This shift toward rational design could reduce development times, improve drug performance, and even make it easier to tailor therapies to individual patients or disease types.
The Broader Picture: Lipid Nanoparticles in Modern Medicine
Before this study, most people became familiar with LNPs during the COVID-19 pandemic, when they enabled the delivery of mRNA vaccines. But LNPs have been around for decades. The first FDA-approved LNP-based drug, Onpattro (patisiran), treats a rare hereditary disease called transthyretin amyloidosis by delivering small interfering RNA (siRNA).
LNPs have since become one of the most promising delivery systems for RNA therapies, CRISPR gene editing, and cancer immunotherapy. Their appeal lies in their ability to protect fragile genetic material and deliver it safely into cells without using viruses.
However, one of the biggest challenges has always been variability—different formulations behave differently, and small changes in composition can dramatically affect performance. The new findings explain why: the internal structure and shape of LNPs have a direct impact on how they function.
How Scientists Could Use This Information
The methods developed in this study—particularly the combination of SV-AUC, FFF-MALS, and SEC-SAXS—offer a toolkit for deeper nanoparticle analysis.
While some of these tools (like synchrotron SAXS) require specialized facilities, others are widely accessible and can be used by research labs and biotech companies.
By building large datasets that link structural characteristics to biological outcomes, researchers could eventually train artificial intelligence models to predict optimal nanoparticle designs for new drugs.
Imagine being able to input a desired therapeutic goal (say, targeting brain tissue) and instantly receive a recommended LNP blueprint. That’s where this research could lead.
What Comes Next
The study provides a blueprint for the next generation of nanoparticle research. The next steps include:
- Expanding the dataset by testing more lipid compositions and payload types.
- Understanding why certain structures perform better in specific cells or tissues.
- Developing accessible versions of these analytical tools for routine use in labs.
- Exploring how manufacturing scale-up affects structure and consistency.
Eventually, this could lead to a world where nanoparticles are engineered with the same precision as the drugs they carry—turning them from passive carriers into active, customizable components of therapy.
The Takeaway
This research fundamentally changes how we understand lipid nanoparticles. They’re not uniform little spheres; they’re complex, diverse, and tunable systems whose structure dictates their performance.
By mapping how shape, composition, and preparation method affect delivery, scientists can now begin designing nanoparticles as carefully as they design the medicines inside them.
It’s not an exaggeration to say that this could reshape the landscape of gene therapy, vaccine development, and personalized medicine in the coming years.
Research Reference:
Elucidating lipid nanoparticle properties and structure through biophysical analyses, Nature Biotechnology (2025)