A New Calculator Could Transform High Blood Pressure Treatment
High blood pressure, also known as hypertension, remains one of the most pressing health problems around the globe. Affecting an estimated 1.3 billion people, it is often referred to as a silent killer because it rarely causes symptoms until it triggers serious complications like heart attacks, strokes, or kidney disease. Alarmingly, fewer than one in five people with hypertension worldwide have their condition under control. This has made the search for better treatment strategies more urgent than ever.

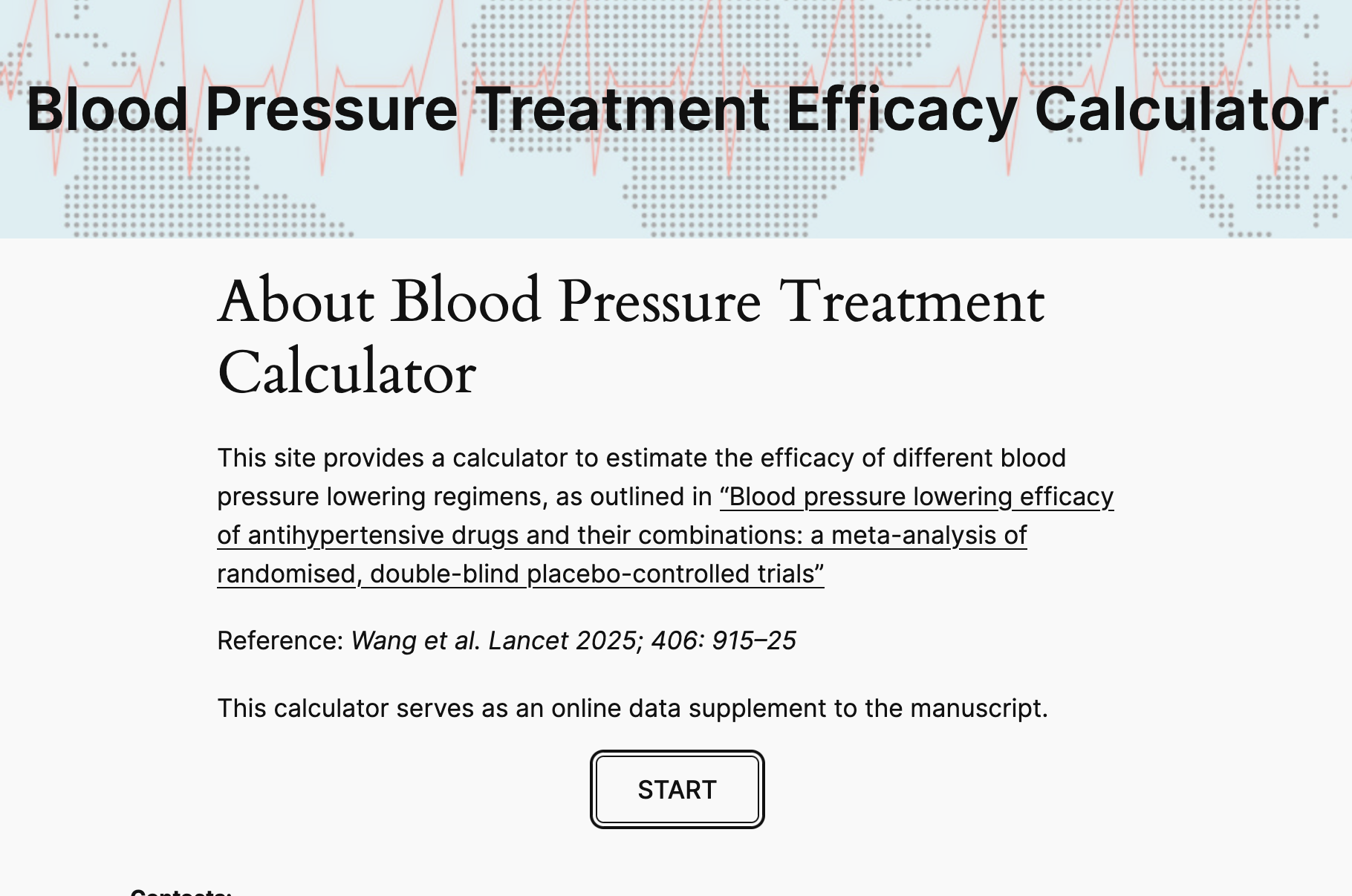
Now, researchers have unveiled a new online calculator designed to predict how much different blood pressure drugs, alone or in combination, can lower blood pressure. This tool, called the Blood Pressure Treatment Efficacy Calculator, is based on data from nearly 500 randomized clinical trials involving over 100,000 participants. It provides doctors with evidence-based predictions that could make hypertension care far more effective.
Why This Calculator Matters
Traditionally, managing high blood pressure involves a step-by-step approach: start with one drug, often at a low dose, then check blood pressure readings, and make gradual adjustments if needed. While this seems logical, it has major flaws. Blood pressure fluctuates naturally from moment to moment, from day to day, and even by season. On top of that, measurement techniques are not always perfect. As a result, blood pressure readings are often too noisy to reliably show whether a particular drug or dose is truly working.
Doctors are faced with a dizzying set of choices. There are dozens of blood pressure medications, multiple dose options for each, and many patients require two or more drugs to reach healthy levels. This means there are thousands of possible combinations, and until now, no clear way to compare their expected effectiveness.
The new calculator directly addresses this challenge. Instead of depending solely on fluctuating readings from a patient’s arm cuff, it uses data pooled from hundreds of carefully controlled clinical trials. By doing so, it estimates how much each drug—or combination of drugs—is likely to lower blood pressure.
What the Research Shows
The findings behind the calculator were published in The Lancet. Researchers systematically reviewed and analyzed data from 484 to 500 randomized, double-blind, placebo-controlled trials, covering the five main classes of antihypertensive drugs:
- ACE inhibitors
- Angiotensin II receptor blockers (ARBs)
- Beta-blockers
- Calcium channel blockers
- Diuretics
From this massive dataset, researchers built a meta-regression model to predict systolic blood pressure (SBP) reductions. The results reveal some important patterns:
- A single standard-dose drug reduces SBP by about 8.5 to 9 mmHg on average.
- Doubling the dose only adds a modest benefit, lowering SBP by around 1.5 mmHg more.
- Two drugs at standard doses can reduce SBP by about 15 mmHg.
- Two drugs at double doses offer an additional drop of roughly 2.5 mmHg.
- Higher starting blood pressure predicts a slightly greater drop: every 10 mmHg higher baseline SBP adds about 1.2 mmHg extra reduction.
The researchers categorized drug regimens into low, moderate, or high intensity depending on the size of the expected blood pressure drop:
- About 72% of single-drug regimens fell into the low-intensity category.
- Around 59% of two-drug combinations were moderate intensity.
- Roughly 11% of dual-drug combinations reached high-intensity levels.
These findings are critical because many patients need drops of 15–30 mmHg to reach target blood pressure goals, meaning single-drug therapy is often insufficient.
How the Calculator Works
The Blood Pressure Treatment Efficacy Calculator is now available online at bpmodel.org. Doctors (and researchers) can input information such as:
- The medications being considered
- Their dosage levels
- The patient’s baseline systolic blood pressure
The tool then provides an estimate of how many mmHg the chosen therapy is expected to lower blood pressure, along with a classification of treatment intensity.
By using this approach, clinicians can move away from the traditional “start low, measure, and adjust” method. Instead, they can choose a therapy plan based on the actual level of reduction required, start it sooner, and adjust less reactively.
Implications for Global Health
The potential of this tool is enormous. Since even a 1 mmHg reduction in systolic blood pressure reduces the risk of heart attack or stroke by about 2%, optimizing therapy selection could save countless lives.
If global hypertension control were raised to just 50%, experts estimate that millions of premature deaths could be prevented each year. In that sense, even modest improvements in how doctors prescribe and combine drugs could translate into major public health gains.
The next step for the calculator is real-world testing. Researchers plan to run clinical trials where patients’ treatments are guided directly by the tool, rather than relying on conventional methods.
Why Blood Pressure Control Is So Challenging
To appreciate the value of this new tool, it helps to understand why high blood pressure is notoriously difficult to manage.
Natural Fluctuations
Blood pressure isn’t fixed—it changes constantly depending on activity, stress, temperature, time of day, and even the season. A patient could measure at 145/90 mmHg one morning, and then show 130/85 mmHg the next day without any medication changes.
Measurement Limitations
Blood pressure monitors, whether in clinics or at home, can be affected by factors such as cuff size, patient posture, and even how long the patient rests before measurement. Small inconsistencies add up, making it hard to assess the true impact of a treatment.
Treatment Inertia
Doctors sometimes hesitate to make big treatment changes when readings fluctuate. This can leave patients stuck at suboptimal blood pressure levels for too long, increasing risk.
Complexity of Choices
With multiple drug classes, each having different mechanisms, side effects, and interaction profiles, choosing the right combination quickly becomes overwhelming. This is where the calculator offers clarity.
Broader Context: How Hypertension Is Treated Today
The standard of care usually starts with one of the main classes of drugs. Each has strengths and limitations:
- Diuretics help the kidneys remove excess fluid and are effective in many patients, but can cause electrolyte imbalances.
- ACE inhibitors and ARBs are widely used and protect the heart and kidneys, but can sometimes cause cough or kidney issues.
- Calcium channel blockers relax blood vessel walls and are particularly useful in older patients.
- Beta-blockers reduce heart rate and workload, often reserved for those with coexisting heart disease.
Most patients eventually need two or more medications to control blood pressure effectively. However, knowing which combination will work best has always been a guessing game.
The new calculator could make this process more rational and less dependent on trial-and-error.
What This Means for Patients
For patients, this tool has several potential benefits:
- Faster results: Instead of weeks or months of incremental adjustments, patients may reach target blood pressure sooner.
- Personalized care: Treatment can be tailored not just to the patient’s current readings, but also to the level of reduction needed.
- Improved outcomes: More patients could achieve blood pressure control, reducing the risk of serious cardiovascular events.
That said, real-world adoption will depend on validation through clinical trials, as well as acceptance by healthcare providers worldwide.
Looking Ahead
The Blood Pressure Treatment Efficacy Calculator represents a major step toward evidence-based, data-driven hypertension management. While it won’t replace the need for clinical judgment, it offers a powerful new way to guide decisions.
Considering the enormous global burden of hypertension—responsible for around 10 million deaths annually—even incremental improvements in care could have profound impacts.
The release of this tool also reflects a broader trend in medicine: moving away from guesswork and toward solutions that integrate large-scale evidence directly into clinical practice.